Thrombophilia: Clinical overview and impact on patients
Brought to you by
Prof. Cédric Hermans, Head of the Division of Hematology, the Hemostasis and Thrombosis Unit and the Hemophilia Center of the Saint-Luc University Hospital in Brussels, Belgium
Prof. Sabine Eichinger, Hematologist, Head of the Coagulation Clinic at the Medical University of Vienna, Austria
Please note:
HEMOSTASIS CONNECT podcasts are designed to be heard. If you are able, we encourage you to listen to the audio or watch the video, which includes emotion and emphasis that cannot be grasped from the words on the page. Transcripts are edited for readability. Please check the corresponding audio before quoting in print.
Tonke de Jong
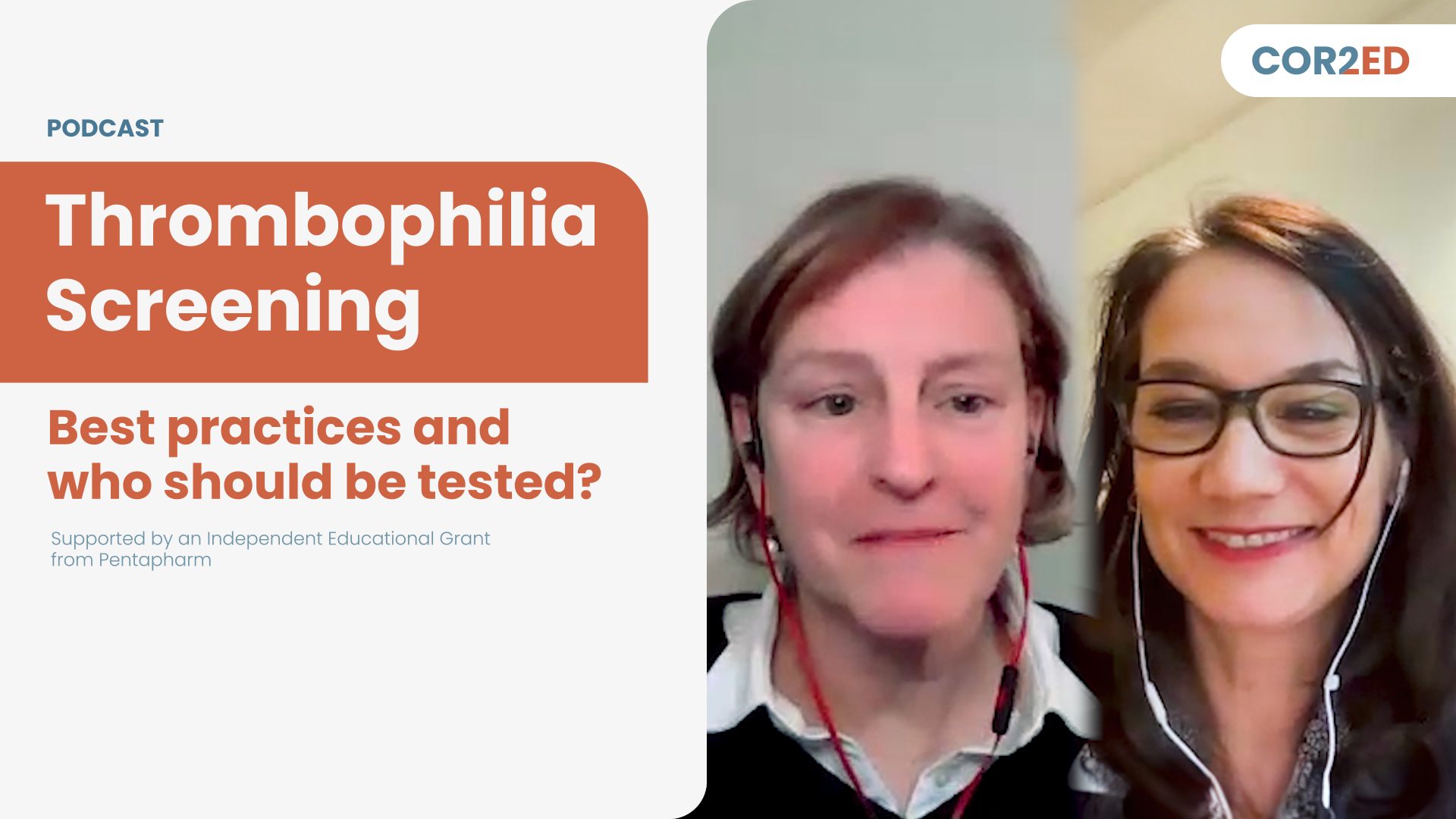
Thrombophilia is a disorder where the body tends to form blood clots, even without injury, and it is associated with an increased risk of thrombotic events. Is thrombophilia acquired or inherited, and what do you know about thrombophilia? Listen to find out more. This is part one in a two-part podcast series on thrombophilia. In this discussion the experts will explore thrombophilia including the pathophysiologic mechanisms and the impact it can have on patients’ lives.
This podcast is an initiative of COR2ED and supported by an independent educational grant from Pentapharm. I’m honoured to introduce to you today’s two experts; Prof. Cedric Hermans who is head of the Division of Hematology, the Hemostasis and Thrombosis Unit as well as the Hemophilia Centre of the Saint-Luc University Hospital in Brussels, Belgium.
And Prof. Sabine Eichinger who is head of the Coagulation Clinic at
the Medical University of Vienna, Austria and she works on thrombosis and hemostasis research. We are very excited to listen to your discussion.
Prof. Cedric Hermans
Dear colleagues, dear friends, it's a great honour and privilege to welcome you to this podcast that will focus on a very important topic, in fact, which is thrombophilia. My name is Cedric Hermans. I'm a Professor of Hematology and heading the Division of Hematology, as well as the Hemostasis and Thrombosis unit at the clinic, University of Saint-Luc, which is one of the major faculty hospital here in Brussels, Belgium. And to discuss this important topic, I have the pleasure to welcome to you Professor Sabine Eichinger. Sabine, maybe you could introduce yourself.
Prof. Sabine Eichinger
Thank you very much, Cedric. It's a real pleasure to be here together with you and to talk about the importance of thrombophilia. and I am a Professor in the field of hematology at the Medical University of Vienna. And, I am head of the coagulation clinic there. And, yes, so many patients suffer from thrombosis. And everybody is, of course, interested in finding out why the thrombosis happened and what can be done to prevent it. So let's see, maybe thrombophilia is the key. Let's see if this holds true Cedric.
Prof. Cedric Hermans
Well, yes, I think this is an important question. You know, I'm really interested in thrombosis, hemostasis. I have to admit that, nearly 70% of my patients are referred because of past thrombotic events, and many colleagues ask us about, you know, finding out the reason for this. Clearly, thrombophilia comes on the table and we get many, many requests to evaluate whether a thrombophilia screening is needed. I'm sure that yourself, in your own practice, you are facing the same challenge, and well, Sabine, I think you agree with me, there are many, many guidelines around. These guidelines are regularly updated. They come from different societies. And although these guidelines well, they provide us with some guidance. My impression is that sometimes they do not help us that much. Would you agree with me?
Prof. Sabine Eichinger
Yes, that's probably, the issue with guidelines, particularly when the evidence is not as strong as we wish it would be, particularly when it comes to really strong recommendations. So, if you do not have enough evidence, then of course, you cannot come up with a strong recommendation. And so particularly in the field of thrombophilia, this is what many people are looking for. So, to really come up with when to test, in which clinical scenario you should test, whom to test. Yes it's a tricky situation.
Prof. Cedric Hermans
Yes. And also you know let's be honest, you know thrombophilia encompasses a very broad family, a large variety of, blood clotting abnormalities. And for those of you who are a little bit less familiar with this, so maybe, let's list them. So one of the most common one, certainly in this part of the world, in Western Europe, is what we call the activated protein C resistance, which is the Factor V Leiden, which is very common. We'll come back to that. And then also another genetic abnormality, quite common too, which is the prothrombin mutation. And we'll come back to this, two major thrombophilia later during this discussion. And then we should not forget several key physiological inhibitors of coagulation. Usually I call them the brakes, the physiological brakes of the coagulation. These are antithrombin protein C, protein S.
And some patients need to be tested for them. And also a large family of specific, blood clotting abnormalities that are the antiphospholipid antibodies. And we know that among these antiphospholipid antibodies with again several potential blood abnormalities; the lupus anticoagulant and then different antibodies the anti-cardiolipin antibodies and the anti-beta-2 glycoprotein 1. So, I think these are the main thrombophilia, these are the main thrombophilic abnormalities that we would screen for I know that there might be others, but I think that the other ones and Sabine maybe you would agree with me - the other ones are probably less relevant.
Prof. Sabine Eichinger
Yes, I completely agree. Other ones are less relevant, either because there has not - the association with, particularly venous thrombosis has never been really established or there are methodological issues. Maybe I can add a little bit on what you just listed before, the different thrombophilic defects. We can, divide them into genetic defects. So those who are inherited and they can also be passed on to the next generation and those who are acquired, which are the antiphospholipid antibodies for example. Whereas for example, Factor V Leiden, the prothrombin mutation and the natural inhibitor deficiencies are all genetic mutations and can be inherited. And of course, there are also differences in the frequency. So, we have frequent thrombophilic defects and we have less frequent thrombophilic defects. So for example, as Cedric, you said already, Factor V Leiden is fairly frequent, at least in our part of the world. And whereas, deficiency of the natural inhibitors, for example, antithrombin deficiency is much, much rarer. And this is important because the rare mutations, they have a little bit more impact on the thrombotic risk than the frequent defects like Factor V Leiden or the prothrombin mutation, which have much lower and less dramatic impact on the thrombotic risk. Yes. And I think you are completely right. And, well, we should all be well aware of the implications of these thrombophilic abnormalities. They do increase the risk of thrombosis. And we will discuss this later on. That could be arterial thrombosis, that could be venous thrombosis. And also when thinking about from thrombophilia, we need to consider whether we are thinking about the thrombotic abnormalities that may run in the family. So that would be genetic ones or other ones that could be acquired and non-existing in the family, like the antiphospholipid antibodies. And while clearly all these thrombophilic abnormalities result in some patients in thrombosis. But it's clear that the thrombosis will be totally different. And we will discuss this later on. So maybe what we could do, Sabine, first is to discuss the implications of these thrombophilic abnormalities in patients presenting with venous thrombosis.
Prof. Sabine Eichinger
Yes, I think this is very important because the relevance of the thrombophilic defect is of course in the venous system. So there is, almost no impact of the classic thrombophilic defects, particularly not the genetic ones on arterial thrombotic events, with one exception, antiphospholipid antibodies. They may also increase the risk of arterial thrombosis. But all the others are if at all, relevant when it comes to venous thrombosis.
Prof. Cedric Hermans
Well, although, you know, I agree with you, but some of these abnormalities like the antiphospholipid antibodies, they might be associated with both arterial and venous.
Prof. Sabine Eichinger
Oh yes. Of course. Of course. they not only are associated with arterial thrombosis but also with venous thrombosis, which makes them sort of unique because they can do both.
Prof. Cedric Hermans
And it's as you already emphasized, while their frequency is highly variable, we know that - well, at least in my region, in my area, antithrombin deficiency, and I think this is true across Europe is quite unusual. By contrast Factor V Leiden is much more frequent. So I think we also need to take this into consideration. And clearly also when thinking about protein C, protein S deficiency, these are not that frequent thrombophilic abnormalities.
Prof. Sabine Eichinger
And also you mentioned something very important before. So this is these are inherited disorders. So you have to really look into the patient family history because there you see if there is a familial tendency towards venous thrombosis. And these are the patients where you really might find some of these genetic disorders and where it might be kind of useful to look closer, and maybe do some testing for the specific alterations to a specific defect.
Prof. Cedric Hermans
Fully agree. I think the family tree is key in our practice. And this is true for patients presenting with bleeding problems, but also patients presenting with thrombosis, and especially when considering who could potentially benefit from a thrombophilia screening or try to identify who, well, what sort of thrombophilic abnormalities might be running. I have several families with, antithrombin deficiency, and when you look at the family tree, there are so many members of the of these families that had thrombotic events in the past. So clearly the penetrance of thrombotic complication is sometimes so high that it makes you suspect that kind of, very severe thrombophilic abnormalities. So let's maybe now move to the screening. So I think screening is important. We need to consider screening. But at the same time, we should not over-screen, we should not under-screen. And, well, I think that I've learned a lot during the last two decades, because this is not easy to know when you do it, when you don't do it. In my view, there is sometimes a little bit of a subjectivity. Some patients might be more better candidates than others just because, and I think this is very important, you need to think about what the real implications are of doing this. So it's easy to tick all the boxes on the form and request all these tests. But I think what's very important is really to think about, will this really impact on the management of the patient, the way I will treat the patient, and will this also impact on the patient himself as a human being and also on the rest of the family? And I think from that respect, having a very open discussion with the patient about, you know, why we do this and what could be the implication is, in my view, important. Would you agree with me?
Prof. Sabine Eichinger
Yes, definitely. I mean, human beings are curious by nature, and this is a good thing, and so this is true for physicians. This is also true for the patient. We want to know why. Why is something like it is. Why did it happen? And so if, there is the opportunity to find something, then, of course, curiosity is always on the top of what we are doing. You have to think it through until the end. With keeping the question in mind, is there anything which is of benefit for the patient once I have the result? Will I change the treatment? Will it change what I'm recommending to the patient? If the answer is no, then you should avoid testing because then you avoid either overtreatment or you avoid undertreatment, both of which are harmful or may be harmful to the patient. In this respect, we have also to keep in mind that venous thrombosis is not due to one single defect, one single risk factor. You mentioned families with, for example, inherited antithrombin deficiency. But even in these families, in the family members who may have a really strong thrombophilic defect in the coagulation system, the thrombosis does not occur solely because of this defect. There are many, many other risk factors which contribute to the thrombotic risk: increasing age, surgery, immobilisation, severe infections, pregnancy, hormone treatment in women, oral hormonal contraceptives, and so on and so on. And you always have to keep this also in mind. So there are a lot of things to consider. And thrombophilia, thrombophilia screening is only one minor aspect in this whole scenario.
Prof. Cedric Hermans
I fully agree with you because, you know, it’s a little bit like a puzzle. There are so many pieces. There are so many risk factors for thrombosis, so many that we need to consider all of them. And I fully agree that we should not consider that thrombophilia itself is the measure or the most important risk factor for thrombosis. It’s one of the many, many that are either related to the patient because of their lifestyle, anatomy, whatever, or because of, you know, surgery they had, ageing, pregnancy, whatever. But that means that we need to list and make sure that we go through all these risk factors before deciding whether a thrombophilia screen is needed. I think this is this is very important. In most hospitals in 2023, thrombophilia screen is possible, is feasible. The tests have been extensively validated. So the tests are there. It’s not that difficult to have access to them. The situation was slightly difficult 10, 15 years ago because at that time some of these tests were quite new. But today you can request the prothrombin mutation assay for protein C, protein S, more or less easily. And I think that also makes you know that the beauty of our discipline is to really decide with the patient if they are a good candidate for this kind of testing. I fully agree with you.
Prof. Sabine Eichinger
And there is also another, another pitfall or another twist in our thinking. So with, because these thrombophilic tests are easily available and because of the progress, which had been made over the last 2 or 3 decades in discovering new thrombophilic defects, we now have the impression that, we know everything. So we can we discovered many, many defects. We have the tests readily available. So we think now we know everything. But that's not true. We need to consider that there might be other, even genetic defects in our system, not necessarily in the coagulation system, which increases, intrinsically, the risk for venous thrombosis, for example. I always give the example that we do not know enough about the role of the venous wall when it comes to, the risk of venous thrombosis. So the venous wall, the endothelium is most likely a major source for discovering new risk factors, new conditions which make patient more susceptible to becoming or to getting a venous thrombotic event. So we have to focus also on the fact that, even if we do not find a thrombophilic defect that there might be something in the patient, might be some unknown defect which we did not yet discover, but which makes the patient at risk for venous thrombosis. So even if we if the thrombophilia testing comes out negative, this is also not the definite answer that everything is fine and nothing is wrong with this patient. And this is a big pitfall in counselling our patients, in adjusting treatment and deciding on the optimal therapy for a patient.
Prof. Cedric Hermans
Yes, I think you are completely right. And now thinking about some families where clearly many members presented in the past with different kinds of thrombosis. And, you know, we perform in these patients all the test we could do and we couldn't identify something which is currently known. So it's clear that in some of these families, there is something genetically present that has not yet been identified. And we need to make sure that we keep an eye on this family, and maybe they will be quite useful in the future to identify new variants. So this is clear, and I also appreciate your comment about yes, we should think about this clotting factor, these inhibitors, the antiphospholipid antibodies. But yes the vessel wall seems important. But also that the cells that are in the blood. We know that the red cells, the white cells we know that some patients present with their thrombosis at unusual location because they have some sort of minor proliferative disease, hyperactive platelets, red cells, things like that. So restricting everything to this Factor V/ prothrombin mutation, I think this is certainly not the way to go. We need to have a very broad view on this. It is very important. And maybe a last concept that we did not emphasize, maybe enough so far is the fact that these most of these thrombophilia are they are predisposing factors. So they are not really the causing factor. So that means that they do exacerbate the major thrombotic influence of several acquired or genetic risk factors. So it's very likely that someone who has a thrombophilic abnormality might be at higher risk in some situation. So it's not thrombophilia itself, but it's from thrombophilia plus something. So it's some sort of equation, you need thrombophilia, you need to add to thrombophilia something in your life that could be hormonal treatment, that could be pregnancy, that could be surgery, cancer, whatever. And all together that will result in the formation of a clot. So clearly thrombophilia is not the reason itself is just making more favourable, I would say.
Prof. Sabine Eichinger
Yes, this is the reason why we have this common expression that the venous thrombosis is a multifactorial disease. And this is, of course, just an expression, just some form of wording. But, in fact it says it all, it's not only one risk factor, not a single condition, but a combination of risk factors, conditions at a certain time point in the life of a patient. So it's risk factors, conditions, time and all this combines and sometimes this combines to the disadvantage of the patient, and then thrombosis might happen.
Prof. Cedric Hermans
But also one of the real added value of this thrombophilia screening some patient is the fact that, let's say you identify in the family that Factor V Leiden is present and seems to be highly penetrant, meaning that many members of the family who have this variant do present with thrombosis. I think that family screening for some specific people could be useful. You know, I am thinking about, you know, young women, who might be pregnant, who might be on the pill. In my view, it's important to screen them before. So family screening in patients who do not have a personal history of thrombosis can be relevant. I think we need to identify the right candidates for this sort of family screening. Would you share the same view in your practice in Vienna?
Prof. Sabine Eichinger
Yes, particularly when it comes to antithrombin deficiency, because antithrombin deficiency really conveys a strong thrombotic tendency particularly. And it really is a familial condition. Yes, where we have many, many family members with antithrombin deficiency, with venous thrombotic events and, particularly in those, who did not yet have, have been a venous thrombotic event, but are carriers of, antithrombin deficiency, you really can advise them better in when it comes to the question of thromboprophylaxis in certain risk situations, when it comes to, contraceptive, mode of contraceptives, when it comes to pregnancy. And this, of course, makes a difference for the patients and also other situations, for example, antiphospholipid antibodies in women when they have miscarriages or when they had, thrombosis, particularly at a young age, you might consider screening for or looking for antiphospholipid antibodies. Because this again may have implications and also implications when it comes to choosing the right anticoagulant, because we know that, direct oral anticoagulants are not to be considered in patients with antiphospholipid antibodies who had already a thrombotic event. So you need to discuss with the patients to switch them to a vitamin K antagonist. And this of course also has implications for the patients.
Prof. Cedric Hermans
Yes I fully agree especially for antithrombin deficiency as well as severe thrombophilic abnormalities. Okay, so time is running. I think that we still have a few minutes left, so maybe, I would like to emphasize a few, additional aspects. The first one is certainly to make sure that, that will be covered in another podcast that we perform this thrombophilia screen at the right time. Make sure that there is no analytical interference or interference with anticoagulants. Also, let's make sure that patients did not have already this kind of test in the past, because avoiding, duplication is important. Some of these tests are quite costly.
I think it's also important to provide the patients with a good summary explaining exactly what they have and good information, I think now there are plenty of good information around so that the patients do not need to go on Google and try to find out some information. We try in my in my centre, we really provide them with information sheet that are really detailed about, you know, what are the implications. Because what we do not want to do is give these patients the impression that they have a new illness. Having thrombophilia does not mean that you have an illness. You just have some sort of genetic variant that could predispose you to some kind of thrombosis. I think these are important aspects, and I hope that our colleagues listening to us agree with this, but do you on your side?
Prof. Sabine Eichinger
I can only emphasize this. I mean, if you are a carrier a heterozygous carrier of Factor V Leiden, for example, you do not have a defect. You are not a patient per se, just because you are an otherwise asymptomatic, human being with a heterozygous Factor V Leiden mutation. And this, needs to be seen with very much caution that you do not make a patient out of an otherwise healthy, individual just because you are running thrombophilia tests, and then you get a lot of results with scary comments.
Prof. Cedric Hermans
Thank you. Well, I think we will soon conclude. So I hope that you enjoyed this podcast on thrombophilia and very open discussions. I think reflecting nicely our practice, try to, you know, integrate the different guidelines and, making the best value of this thrombophilia screen. I think they are important. I think, thrombophilia screen was not possible 50 years ago. Now it's possible, it's really helping the patient and, I think we need to value them as much as we can. And maybe, Sabine, you could conclude yourself with some final words for our colleagues.
Prof. Sabine Eichinger
Sure, Cedric. It was, a real big pleasure, and I enjoyed it very much, talking to you about this very important topic. And let me emphasize once more, all of us think it through, ask if the result has any clinical benefit for the patients or the relatives. In the end, avoid over-treatment and under-treatment just based on the result of the thrombophilia testing.
Prof. Cedric Hermans
Thank you. Thank you Sabine. Thank you.
Prof. Sabine Eichinger
Thanks to the listeners. It was a pleasure.
Prof. Cedric Hermans
It was a pleasure for me too. Bye bye. See you soon.
Prof. Sabine Eichinger
Bye bye.
Tonke de Jong
Thank you so much for this interesting discussion. We’ve learned a lot about the causes of thrombophilia, how to identify patients at high risk and implications of the disease on the lives of patients.
If you enjoyed this and want to find out more on thrombophilia, then please look for the other episodes on the “Hematology Medical Conversation” under the account of COR2ED medical education. Also don’t forget to rate this episode or inform your colleagues about it. Thank you for listening and see you next time.
This video podcast is an initiative of COR2ED and developed by HEMOSTASIS CONNECT, a group of international experts working in the field of hemostasis. The views expressed are the personal opinions of the experts. They do not necessarily represent the views of the experts' organisations, or the rest of the HEMOSTASIS CONNECT group. For expert disclosures on any conflict of interest please visit the COR2ED website.






 Downloadable
Downloadable  6 MIN
6 MIN
 Dec 2025
Dec 2025