Please note:
NET podcasts are designed to be heard. If you are able, we encourage you to listen to the audio, which includes emotion and emphasis that cannot be grasped from the words on the page. Transcripts are edited for readability. Please check the corresponding audio before quoting in print.
NET CONNECT is an initiative of COR2ED. This podcast is supported by an educational grant from Ipsen. The views in this podcast are the personal opinions of the experts. They do not necessarily represent the views of the experts' organisation or the rest of the NET CONNECT group. For experts' disclosures on conflict of interest, please go to Oncology on www.COR2ED.com.
Dr Aman Chauhan:
Welcome to this podcast. The role of somatostatin analogues at progression to continue or not. Today we will cover clinical practice points, data to support clinical decision making and patient impact of switching treatment or continuing SSA in progressive patients. My name is Aman Chauhan, I'm one of the medical oncologists at University of Kentucky with a clinical and research interest in neuroendocrine cancers. And I currently direct our theranostics programme at Markey Cancer Centre. Today I have the good fortune to have with me Professor Martyn Caplin from England. He is a tour de force in neuroendocrine tumours, lead investigator of CLARINET trials and several other studies. Martyn, over to you. Would you like to introduce yourself to our newer audience? I know you don't need any introductions, but for the new folks listening in.
Prof. Martyn Caplin:
Well, it could be, I'm so old, they don't even know of me. So, it's good to be here. Thank you very much, Aman. So, I'm Martyn Caplin and I'm Professor of Gastroenterology and Neuroendocrine Cancer at the Royal Free Hospital in London and at University College London. And I lead the ENETS centre of excellence here for neuroendocrine tumours.
Dr Aman Chauhan:
Wonderful. Thank you, Dr Caplin, for being with us. So before we go into deeper aspects of our topic today, let me prime the audience briefly with somatostatin analogues. Now somatostatin analogues have been used for several years, actually a few decades in neuroendocrine oncology. But the biggest seismic shift that we have seen was use of long-acting somatostatin analogues, which are now the backbone of the treatment, I would say the mainstay of the treatment for metastatic neuroendocrine cancer patients. Currently there are two major products, lanreotide and ocreotide LAR in the US, and they're used interchangeably for both disease control as well as carcinoid syndrome and function-led control inherent in neuroendocrine tumours. Today we will discuss some of the pivotal studies that led to the clinical use of these agents. But the key question today in front of us is: at the time of progression on SSAs, is there a role for continuing somatostatin analogues at progression? And if yes, what data would support that? With that introduction, over to you Martyn. Give us a brief introduction about strategies that you personally use in the European set up and kind of abreast us with the current guidance from ENETS regarding this particular hot topic.
Prof. Martyn Caplin:
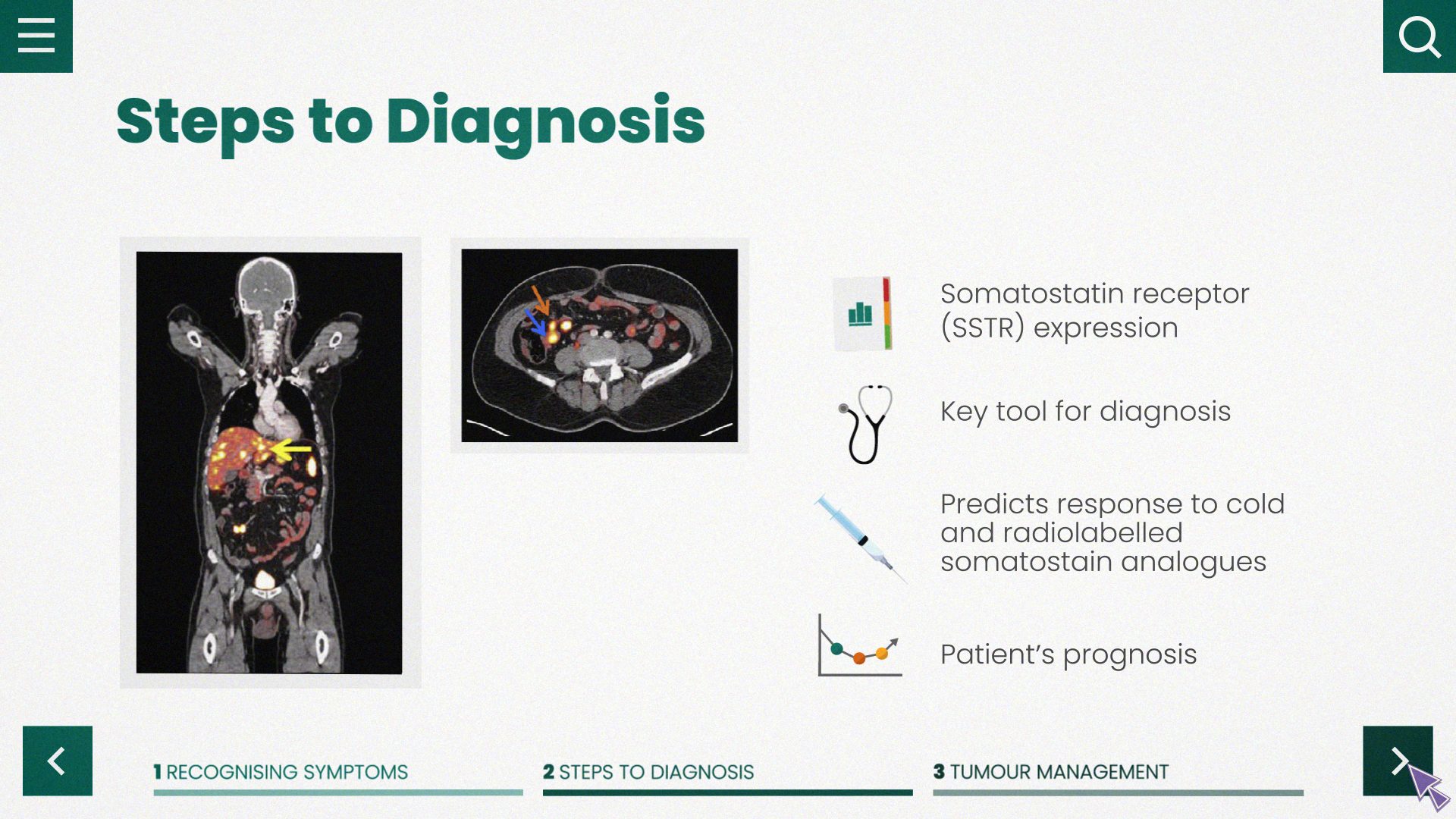
Thanks very much Aman. I suppose when you're assessing what treatment you're going to give any patient, you'd look to see one, whether or not they're syndromic or not, the type of neuroendocrine tumour they have, mid-gut, pancreatic or bronchial for that matter, the volume of disease that they've got, the rate of progression. I think you'd want to understand the biology of the tumour, well-differentiated tumours versus poorly differentiated, and within the well-differentiated their grading of Ki-67. And of course the imaging, not only in terms of volume of disease and rate of progression, but obviously whether they've got somatostatin receptor positivity for example, with a gallium 68 somatostatin analogue PET scan. So one takes all of that into account.
For today's discussion. We're essentially talking about the well-differentiated grade 1, grade 2 neuroendocrine tumours and in the context of slow progression and the use of somatostatin analogue in that situation. And we know from the original PROMID study and of course the CLARINET study, primarily with octreotide LAR in mid-gut neuroendocrine tumours, CLARINET in predominantly mid-gut and pancreatic neuroendocrine tumours, also some mid-gut, the anti-tumour effect of both octreotide LAR and lanreotide autogel. I suppose if I was going to be contentious at the beginning, we know from PROMID and from lanreotide, I'll come on to the rest of it, we're having a wee bit of a discussion here, but, you know, in the early days, you used to start off at 20 milligrams of octreotide LAR. And now because of PROMID, everyone starts off at 30 milligrams and similarly lanreotide, everyone starts off, because of CLARINET, 120 milligrams. Do you think there's still, I'm going to bounce it back to you because we're having a discussion here, but you think there's a role for starting someone on 20 milligrams of octreotide LAR, and then waiting and seeing and increasing that way, and similarly, 90 milligrams lanreotide autogel, or do you think we should, everyone should, be starting at the higher dose?
Dr Aman Chauhan:
Wonderful question, Martyn. I'm sort of relatively newer in the field, and I've seen the current practice pattern, at least in the United States, since we are post PROMID era, I've seen oftentimes you start with either 30, and with lanreotide it's a straightforward 120 dosage. However, there are some patients which I've inherited and from the previous providers who were on 20 and doing great on that. So, I do have that clinical perspective. However, based on the best available randomised data, I think for octreotide LAR, 30 makes me feel a little bit more comfortable considering I have the very superior tumour control data on that dose. Now do I alter with that? Do I go higher than that? That's the question which has come to all of our minds, especially since NETTER-1, which use higher dose octreotide as a control arm, and were able to show some degree of disease stabilisation. I think median PFS, you know, 8 to 9 months or sometime during that range. So flipping the question back to you, what is the role of increasing the dose or frequency of both of these LARs or long-acting somatostatin analogues?
Prof. Martyn Caplin:
So it's interesting. So let's just discuss first line because I suppose in, it was 2009 actually, Christos Toumpanakis was the first author on the paper which we published on octreotide LAR. We had patients on 20 milligrams and if they showed signs of progression and that was around about a year later, they went up to 30 milligrams and they did well. And I was always interested in case you get to that question of tachyphylaxis, because if you start at higher dose, do you perhaps get tachyphylaxis at an earlier stage? But you're right, the standard I think, in Europe now, through the States is actually most people will start with octreotide LAR 30 milligrams and lanreotide autogel, 120 milligrams every 28 days. And I think we agree that that's probably the standard practice, but I just wanted to put it out there that that's only because the trials were done at that, PROMID and CLARINET, and you could argue we don't have the evidence base in a randomised form, but actually we used to start off at 20 milligrams LAR and then go up to 30 milligrams and 90 milligrams going up 120. I don't think there's a role for the ten milligrams LAR or 60 milligrams for that matter of lanreotide autogel. But just to put it out there and in terms of people's thinking, but I think standard practice is the higher dose.
And then so the question is what you do when the new neuroendocrine tumour progresses? So I've already diversified already from your original question, it could be a very long, I promise the listeners it won't be so long, but so you have to then decide, for mid-gut and pancreatic for slowly progressive disease as to say well-differentiated grade 1/grade 2, we'd look to increase the dose of somatostatin analogues. And then the question is, well do you do that by just increasing the dose and going from 120 of lanreotide autogel to 240 milligrams, or do you go from 120 milligrams every 28 days or to 120 milligrams every two weeks? And I don't think there's a right or wrong way. And I think that the Italian study, that didn't show any difference. Similarly, when you're considering the same for octreotide LAR, we know, as you say from NETTER-1, that actually 60 milligrams of octreotide LAR in those patients who had progressive disease was reasonably well tolerated. It's more in the way of diarrhoea, as one might have expected. And that there was a progression-free survival of around about 9 months in that group of patients. So that was good. And in CLARINET FORTE that was 120 milligrams. That was the Marianne Pavel study from 2021 that was published, and that was CLARINET FORTE 120 milligrams every 14 days in mid-gut and pancreatic neuroendocrine tumours. That was a single arm, phase 2 study, and so you saw the benefits there in both progression-free survival was around about 8.5 months in the mid-gut and was less actually in the pancreatic group, it was only
Dr Aman Chauhan:
5.6.
Prof. Martyn Caplin:
Yeah. Because except for that group, of the pancreatic neuroendocrine tumours, was less than 10%. Then you saw a similar result, 8 months there. So that actually also brings into question, well as the if you've got a higher grade, grade 2 neuroendocrine tumour, you’d think that the response actually to the higher dose somatostatin analogues is not going to be quite so long, but actually if it's a G2, up to 10%, actually you'd be expecting a PFS of around about 8 to 9 months. So and some patients do better than that, a few do worse, but I think that would be the way forward from there. And then, the Italian study, as I say, whether it's once every 28 days or once every two weeks, but double the dose. And I don't think there's much difference, whichever way it works most conveniently for the patients and the logistics of it as well. What's your practice?
Dr Aman Chauhan:
So, Martyn, we live in a very interesting era, especially for drug development and neuroendocrine cancers lately. And we have what we call problem of plenty, which is a good problem to have. So, in the past where optimising the dose of SSA was in vogue because, primarily because of lack of treatment options, we now have on-label options for metastatic progressive mid-gut, everolimus; and lutetium, Lu, 177-DOTATATE we have options, sunitinib for pancreatic NETs. We also have some good prospective, randomised data on agents like capecitabine/temozolomide for various subsets of neuroendocrine tumours. So, in context of multiple treatment options, we are seeing that there has been change in the practice patterns where we are no longer obligated to stick around with SSA or this class of drug at time of progression. Having said that, there, I think, has to be a more nuanced approach because as you mentioned, SSA has been around for a really long time, primarily because of convenience of administration, once-a-month injection, safety profile, the patients can stay on it for a significant amount of time without consequential end-organ, bone marrow side effects. So, there are definitely a lot of pros in using SSA said that really propels us to continue using SSA in select patient population at time of progression, especially if patients are relatively asymptomatic. It's a slow progression. Patient does not feel comfortable with the idea of progressing into or trying out cytotoxic chemo or radiopharmaceutical drug or another TKI, which can have significantly higher side effects as compared to SSAs. So, I think the answer lies in a nuanced approach, taking into account the need, the tumour progression, the degree of tumour growth, symptomatology; then we decide whether we continue SSA at a higher dose or a higher frequency or we change the class of agent. I think we both agree that for functional NETs it's pretty standard to continue SSA regardless while we figure out the appropriate anticancer regimen. But our biggest patient population is in non-functional NETs. That's where we have to really discuss the case in a multidisciplinary tumour board, and then kind of really think it through, the pros and cons.
What the studies that you've mentioned, the CLARINET FORTE, for example, have at least given us confidence that there is data to support higher dose or increased frequency of SSA and that can potentially have a role. You know, I was very impressed with CLARINET FORTE, although it's a decent sized single centre, single arm study in 99 patients and definitely showed some, some indications of cytostatic activity in especially the mid-gut population at progression with 8.3 months of median PFS. That's I think for some patients that might be very meaningful, and similarly NETTER-1, placebo or a control group, also reaffirms that there could be added activity at progression for higher dose SSA. So, I think it has to be a little bit more nuanced approach and good to know that there is some safety data to confirm that we can continue SSA at a higher dose or frequency in some select patient populations.
Prof. Martyn Caplin:
Yeah. So I think you can summarise that by saying slowly progressive disease, well-differentiated G1/G2 tumour, moderate, small-to-moderate volume. It's entirely appropriate to go as a second line to increase the dose of somatostatin analogues. I think we're agreed on that. I think on both sides of the Atlantic, and I think the guidelines are heading that way. And certainly the consensus is, on both sides of the Atlantic, that that's the way to go.
Dr Aman Chauhan:
Martyn, if might, if I may add another important point, especially the country, large country like the United States, where majority of patient treatments start out in community, 90% of our cancer patients are treated out in community setting, their access to radiopharmaceutical treatment or clinical trials might be somewhat limited. So, all these agents, which the providers are very comfortable using at higher dose of those at time of progression, can be a very valuable tools in their toolbox while they're trying to get patients transferred to a high-volume tertiary care centre, at same time it might not even be possible because there are no NET centres in the vicinity. So, all-in-all, I think it's a win for the patients that they at least have an option to go higher the dose, or frequency, especially, if they don't have access to the newer treatments.
Prof. Martyn Caplin:
Yes, and I have to say we've sometimes gone in terms of the scheduling from just for example, 120 milligrams every four weeks down to three weeks and then down to two weeks. So, patients have done well doing it that way is as well, providing you're keeping an eye on them and scanning them on a 3- to 6-monthly basis. So, there's no definite sort of way forward in doing that. But I think actually, practically, reducing the frequency seems to work equally well. So, I don't see that as being a problem. I think there's amount of leeway on which you can take this forward. Do you stop though, the somatostatin analogues, you've got a patient with a pancreatic neuroendocrine tumour, they've progressed on their higher dose somatostatin analogues, you're giving them CAPTEM now. Do you stop the somatostatin analogues at that point, if they're not syndromic?
Dr Aman Chauhan:
Just a great question, again. This is one of those things where we truly lack prospective randomised data to guide us. However, my personal practice is to stop SSA in pancreatic NETs if I'm switching them over to cytotoxic chemotherapy, and then for example, CAPTEM can be highly effective just by itself in NETs and the response rates are actually very impressive especially PNETs setting. And so we have to also factor in the financial toxicity and burden added to the patient. I feel with an effective treatment like CAPTEM, and CAPTEM by itself, also very taxing on patients with a very complex 14-day regimen, and they have to come for a monthly check-up for bloodwork, I try to minimise additional therapeutic interventions, unless there is a very convincing data to support that adding SSA would certainly accentuate the benefits. Having said that, if your scenario flipped to PRRT, for example, my practice might be somewhat different. And maybe this is a good segue way to discuss role of SSA during and post PRRT, because my personal practice has swayed from discontinuing SSA to now continuing SSA during PRRT and post PRRT. And then maybe we can have a little powwow regarding that. Martyn, what, let me flip that question to you in context of theranostics.
Prof. Martyn Caplin:
Let's go to back to the chemotherapy one, first of all. I think you're right that if the patients progressed through their higher dose somatostatin analogues, it's totally reasonable to stop it. You go onto your CAPTEM and then the question is, once you've completed your CAPTEM, though, so some people will carry on long term, but other people will stop, for example, after six cycles if they just had got stable disease at that point. And then you have the REMINET. That was where the REMINET study came in in terms of looking at the role of lanreotide autogel, in patients, in that, that was a randomised, double blind placebo-controlled trial after, essentially the chemotherapy that most of those patients had had, should you give them lanreotide, after the chemotherapy or not? And that was that was the placebo group versus the group who had the lanreotide. And undoubtedly what came out of REMINET that was there was a benefit, actually, if you put the patients on the somatostatin analogue after the chemotherapy. So, the median PFS in the active treatment group was 19 months plus and in the placebo with lanreotide that was 120 milligrams, and the placebo group was 7.5 months. So, there was definitely, seems to be a benefit - it wasn't such a small study, there was 50 in each arm. So I think you could argue that that would be reasonable after chemotherapy, to put patients on a somatostatin analogue. The caveat to that, though, is that patients feel quite a lot better coming off their somatostatin analogue because they're not getting the steatorrhoea and the griping abdominal discomfort. And so, you know, I think it's not unreasonable to say, well, maybe come off it, but if you show some signs of progression, we can put you back on a somatostatin analogue at that time. But the answer from REMINET was that actually those patients who’ve had chemotherapy actually did better if they were put back on the somatostatin analogue.
Dr Aman Chauhan:
If I may add, that's a beautiful study that you pointed out, especially our understanding of long-term side effects with CAPTEM, we're understanding the toxicity both short and long term and our practice has been now moving towards more truncated or the shorter versions of CAPTEM. There was a time I used to use CAPTEM at a stretch for a year and a half, maybe at a lesser frequency, now I routinely stop CAPTEM after nine months. So in that context, I do feel with lesser induction regimen CAPTEM, there could be definitely a role of maintaining with a more safer medication like lanreotide, and that REMINET data certainly compels us to think using SSA as a maintenance post CAPTEM.
Prof. Martyn Caplin:
Yeah, and then you can always retreat if they've responded well down the line. I think that that's a very reasonable way forward. Moving on to the PRRT aspect of it, of course, the NETTER-1 study involved continuing the patient on octreotide LAR 30 milligrams in between their courses of PRRT. And I think that's totally reasonable and that would be our practice, actually, to do that in the real world. And I suppose the interesting paper in context of that was the one from a couple of years ago from, was that the Bonn group who published on that?
Dr Aman Chauhan:
That's correct.
Prof. Martyn Caplin:
And that was interesting because it showed that if you, so they divided up, there were two groups it was 80 in one group which just had PRRT alone and 87 in another group which had PRRT plus the somatostatin analogue and the progression free survival in the group which was just PRRT alone without somatostatin analogue was 27 months. But in the group that had PRRT plus somatostatin analogue the PFS was 48 months. So that's very compelling although in good numbers of patients, although it was a retrospective study. But my inclination is actually to actually put patients on, or keep them on, somatostatin analogue during and after their treatment, even if they're non-functional. But again, I have a number of patients who say, you know what, I want to have a break off the somatostatin analogue, and ideally I would like to stop it and because of the side effects. And so those patients do okay for a good period of time. And you have the choice then if there’re signs of slow progression to put them back on somatostatin analogue. Obviously there's a whole question then of retreatment PRRT, which is for another day, but I think that would be a reasonable approach. What do you do in the States? What's your protocol?
Dr Aman Chauhan:
So wonderful question Martyn, and I do agree with you. I think there cannot be a one size fits all approach. A lot of time we factor in the patient preferences if the patient has had it, and wanted some break off the monthly shots, especially after PRRT or during PRRT, that's very reasonable. However, my personal practice has switched from not continuing SSA post-PRRT to routinely continuing SSA, and some of the factors which have led to that has been, of course, the strongest data comes from the Bonn group, which has shown that this single centre study that you mentioned, almost doubling the benefit with the combination, but also my anecdotal experience. So, I'm very impressed with continuing SSA as long as patient is okay and there are no side effects. Having said that, just a small plug. So, me and Simron Singh from CCTG are going to be co-leading NET Retreat Cooperative Group International Study. And one of the stratification factor of the study is the prior use of SSA post PRRT. So, we will try to prospectively look into whether there are signals of added efficacy in patients who continued SSA post initial PRRT. So hopefully we'll have some data coming up to fill this critical unmet need of prospective data looking at the role of SSA post PRRT. But it's a very, very good question. Unfortunately, with no good data. However, my personal practice and most people here in the US do tend to seem to continue SSA post PRRT.
Prof. Martyn Caplin:
Yes, and I think that's probably the case in Europe as well for our general practice, as well. So, I think we even if we even agree on, on that one, om both sides! So I suppose, I'm cognisant aware that we're now running out of time. But I think we've actually sort of come to a situation where for well differentiated, slowly progressive disease it's appropriate to increase the dose of SSTA and whether that's going every two weeks or just doubling the dose, that then with chemotherapy there's an argument following chemotherapy, based on REMINET, that actually patients should probably go back on a somatostatin analogue there and that for PRRT you would continue it during and then afterwards as well, at a standard dose. The other bit about that though, is if a patient's been on, let’s say, 60 milligrams of ocreotide LAR or 240 milligrams of lanreotide autogel, and then they had their PRRT afterwards or chemotherapy for that matter. Would you carry on at that high dose? Would you put them on a standard dose?
Dr Aman Chauhan:
Oh my goodness. That's reminds me of that movie Inception. You know, it's...
Prof. Martyn Caplin:
I said I'd throw you a curve ball question! So, this is it, I saved it till the end!
Dr Aman Chauhan:
Right, so I think that is a fair question because this is a situation which we will soon see on the uptake, with the advent of PPRT-PRRT, we are seeing patients are progressing on PRRT and are being now re challenged with PRRT and other line of therapies. As our patients live longer, we'll continue to have these questions regarding continued role of SSA post second line, third line, fourth line. Having said that, I think we'll have to use the same guiding principles. What are our alternative treatments at that point of time? If we have a reasonable, good third line, either in a clinical trial setting or a standard treatment, is there data to suggest safety of adding SSA to those agents. Patient preference is paramount. If a patient is okay with continuing SSA and how has patient's prior experience with SSA? Has there been pancreatic insufficiency, steatorrhea, and other issues? I think we'll have to continue to navigate these troubled waters with nuance, unless we have some good quality data. I think I am happy with continuing SSA, like you mentioned, post PRRT for the time being; I'm happy, looking at REMINET data, that gives me some justification, using SSA post cytotoxic chemo, especially if I can truncate the chemo regimen and prevent some of those long-term minor toxicity and maintain on SSA; SSAs are relatively safer, long term safety data exist. With that, Martyn, I think we are closing in on our allotted time. Any, any final words, any piece of advice for our listeners?
Prof. Martyn Caplin:
My key take home messages are that for well differentiated G1, G2, neuroendocrine tumours, if there's slowly progressive disease it is entirely reasonable to increase the dose of somatostatin analogue, whether that be increasing the frequency from four weeks down to two weeks or even three weeks or just increasing the dose every month. I think that after second line therapy, such as chemotherapy, there's evidence to suggest the benefit of continuing somatostatin analogue in that group of patients. And similarly for those patients with PRRT, again during PRRT and after PRRT, I think the evidence is there to continue somatostatin analogues.
Dr Aman Chauhan:
I concur with my colleague Dr Caplin and I'd like to add, in neuroendocrine tumour patients who are SSTR positive, we have a wonderful drug with significant safety profile data available and we should be willing to use this if it can help us minimise toxicity, for example, if we can reduce exposure to chemotherapy and maintain patient on SSA. If we can continue SSA maintenance post PRRT, there's some data to really convince us that there is added benefit of adding SSA post PRRT. So, there is a role of continuing SSA post progression, but I would suggest that as a community we need to design studies to really tease out the target patient population so that we can continue SSA in the right patient without over burdening the system and not treating everybody with a shotgun approach.
Prof. Martyn Caplin:
I think it's been a fascinating discussion in terms of the clinical aspects of this and the clinical trials and how, how we use that. So thank you very much for the opportunity to be involved. It's been a great pleasure Aman, to be discussing with you and, and with our audience.
Dr Aman Chauhan:
Likewise. Pleasure was all mine, and I echo Dr Caplin’s comments. this is a very important tool in our toolkit, and we shouldn't really let go, unless we have a really strong reason to not continue SSA post progression. Wonderful to have you here, Dr Caplin, a pleasure to talk to you as always. Learned so much from you and through this interaction. ‘Til we meet again, thank you.
Prof. Martyn Caplin:
Thank you.










 Downloadable
Downloadable  20 MIN
20 MIN
 Feb 2026
Feb 2026