In this key clinical topic presentation, Prof. Sammy Saab shares insights on the differing benefits of immunotherapy in HCC patients with NASH/NAFLD risk factors. Through his video discussion and slide set, you'll learn about treatment sequencing and real-world outcomes in this special patient population.
Hello everybody. My name is Sammy Saab, I'm a hepatologist at UCLA. And on behalf of HCC CONNECT, I'll be talking about response to immunotherapy in hepatocellular carcinoma, focusing on real world experience and the treatment sequencing in a very important population: those patients with NASH/NAFLD. We're going to cover three very important aims during this conversation:
We're going to review the emerging role of fatty liver as a cause of chronic liver disease and hepatocellular carcinoma.
Secondly, we’re going to understand the role of immunotherapy, the treatment of hepatocellular carcinoma, and its potential limitations to efficacy in varied patient populations.
And lastly, equally important, be familiar with sequential therapy for hepatocellular carcinoma.
So, NASH and fatty liver are public health concerns. You know, across the globe we see a prevalence to be 1 out of 4 people. But what’s particularly disturbing is that prevalence varies according to risk factor. You know across the globe we've seen higher rates of diabetes and hypertension, hyperglycaemia, and obesity, and these are driving the risk of fatty liver. In some groups, for instance, the rate of fatty liver can be as high as 1 out of 2 people, particularly people with type 2 diabetes.
Now, the natural history of fatty liver is very interesting; although fatty liver is very, very common, it's only a subset that will develop liver complications. These include fibrosis, cirrhosis, liver failure and liver cancer. It’s only a small subset; the difficult thing we have as hepatologists is recognising who among the fatty liver patients will develop this serious type of fatty liver which we call NASH.
Indeed, across the globe and particularly in the United States, hepatocellular carcinoma with the risk factor of fatty liver appears to be increasing significantly. Please bear in mind that liver cancer does not occur in a vacuum. Liver cancer occurs in a setting of “dirty soil,” whether it be hepatitis B, hepatitis C or alcohol, or fatty liver. And if you look at people waiting for liver transplantation here in the United States, the most common underlying risk factor for liver disease is fatty liver. This is fueling, fueling the rates of liver cancer.
Now we're lucky that we have a number of guidelines, of algorithms to help us with the treatment of liver cancer, but you’re dealing with two diseases: cirrhosis and liver cancer. So, this year the Barcelona Clinic Liver Cancer staging and treatment strategy has become available, and it highlights that the treatment of liver cancer depends on the tumour burden, depends on severity of liver disease, depends on someone's functional status. And in a small subset of individuals with advanced stage liver cancer, who have unresectable tumours, are eligible for systemic therapy.
Now, the approach, the exact treatment decision to deal with liver cancer is best left to a multidisciplinary team. And depending on your institution, this may include one of many interventional radiologists, hepatologists, oncologists, diagnostic radiologists, hepatobiliary and transplant surgeons, and members of palliative care and radiation oncology, and pathologists. So, it takes a team approach because there are a number of options for people who have tumours that are unresectable.
Now, two years ago, Richard Finn and his colleagues published in the New England Journal of Medicine the results of using immunotherapy in combination as first line therapy for liver cancer. They looked at 500 patients and they found a significant improvement of overall survival with atezo and beva over sorafenib. The median progression free survival is 6.8 months with this combination therapy, versus 4.3 with sorafenib. But others have highlighted that the devil's in the details.
This is a very nice paper published in 2021 in Nature, and it highlights that not all patients derive the same benefits from immunotherapy, in those have advanced hepatocellular carcinoma. Pfister and his colleagues performed a meta-analysis of three large randomized, controlled, Phase 3 trials: the immunotherapies in patients with advanced liver cancer. These are called CheckMate459, IMbrave150 and KEYNOTE-240. And they found that overall indeed, indeed immunotherapy improves survival significantly with a hazard ratio of 0.77. And when they looked at subgroups, they found indeed that with viral hepatitis, people did quite well. Their survival was improved over, over the competitor, over the placebo or the control arm. But they found that survival may not be superior to control arm in patients with non-viral liver cancer.
Pfister highlights the meta-analysis of over 1,600 patients and indeed of the overall survival with immunotherapies improve. But when Pfister and their colleagues tried to find data to non-viral and viral, you see a very important finding. Indeed, as I mentioned earlier, viral cause of liver cancer has a significant improvement but non-viral, non-viral the hazard ratio was similar - was close to 1. Highlighting that they may not have the same benefits.On a separate meta-analysis where he further stratified the viral causes, and he teased out hepatitis C, hepatitis B, cause of unknown liver disease associated with liver cancer, and he found that for those two entities; those two entities survival was indeed better with immunotherapy in the control arm, but not for the non-viral liver cancer aetiologies.
Dr. Pfister also looked at another population. He looked at their own patients; he had a test cohort and he looked at 130 patients with advanced HCC and he stratified data according to NAFLD versus other aetiologies, and then adjusted for Child-Pugh score, vascular invasion, performance and AFP levels. And he found in this very elegant, elegant study that patients who had NAFLD have a significantly worse survival than patients who had cirrhosis and liver cancer from other aetiologies. In a validation cohort of 118 patients with also advanced HCC, he found very similar results: that patients with underlying NAFLD had a worse survival than patients with liver disease from other aetiologies. This is very, very concerning.
So, at ASCO GI, we heard from two different authors looking at their own real-world data of response to immunotherapy in patients with liver cancer. One study from UCSD; one from Mount Sinai. And what they have in common is that both confirm, using real-world data experiences, the observation by Pfister and his colleagues that patients with NASH cirrhosis do less well than patients with viral causes of liver diseases.
As you remember the mechanisms of action of checkpoint inhibitors, these work by “turning on the light switch.” Liver cancer cells inhibit the action of CD4+ and CD8+ T cells, and by using checkpoint inhibitors, we turn on the light switch to activate these T cells. Unfortunately, there has been a plethora of data highlighting that in patients' fatty liver the tumour immune surveillance is impaired, and the CD8+ cells do not work as well. So this provides some biologic possibility of why the response differs in a patient with fatty liver versus other causes of (fatty liver) disease.
In terms of overall survival, this is a very nice study highlighting that sorafenib treatment improved overall survival in patients with NAFLD- or NASH-related hepatocellular carcinoma in comparison to patients with viral and alcohol-caused liver disease when used at first line therapy. You see here that the P-value was 0.002.
In a separate study published in 2021, we saw the overall survival with levantinib to be greater in patients with NASH cirrhosis and hepatocellular carcinoma than in patients with non-NASH HCC. Progression free survival was similar between the two groups.
And in this very nice study by Singh et al. published in Future Oncology highlighted that also the real-world effect of the levantinib for hepatocellular carcinoma patients with NASH were similar to the overall cohort of 397 patients.
So, we see that sorafenib, levantinib, the results tend to be better in NASH patients than other populations, or as good as in other populations.
Now the National Comprehensive Cancer Center proposed sequence of treatment of liver cancer starts off with preferred regiment of atezo and beva for people with Child-Pugh Class A cirrhosis. But they also highlight that we have other first-line therapies: sorafenib and levantinib. But they also recommend that if there's progression - which we all know that people with liver cancer are going to experience progression at some point or another - we have a number of other options.
So, in this very nice paper by Pinter published last year is a proposed treatment algorithm for special populations. And basically what I want to focus is there are certain populations that you cannot use immune therapy, like those who have had a solid organ transplant for risk of precipitating rejection, and patients who have pre-existing autoimmune diseases that are not being well-controlled, or inflammatory bowel disease as well.
Another population that needs more study are the patients with NAFLD and NASH. So, right now still atezo and beva are considered first-line therapy. But we have to be prepared because therapy, as you saw earlier, is not as effective in this population as compared to other populations with viral hepatitis as an aetiology of liver disease. And be prepared for that sequence of therapy. And if you decide to use immunotherapy as first line, be prepared for the sequence of therapy. Be prepared to switch them in a short period of time because they tend to see better results than immunotherapy.
So, in conclusion, you know, a major consequence of this epidemic of fatty liver and NASH is increasing incidence of hepatocellular carcinoma, which has been fueled by diabetes, hypertension, hyperglycaemia and obesity. Multi-disciplinary teams are incredibly helpful to determine the appropriate treatment paradigms in patients with hepatocellular carcinoma, and although survival in patients with hepatocellular carcinoma is substantially improved with immunotherapy, their benefits may not be equally realised by all patient groups. And patients and clinicians must be prepared for sequential therapy, when patients are treated for hepatocellular carcinoma, particularly those with underlying non-alcoholic fatty liver disease.
Well, thank you for your attention. Please feel free to download the slides. And on behalf of HCC CONNECT, have a nice day and again, thank you for participating.
Sammy Saab, MD is a Professor in the Departments of Internal Medicine and Surgery at the David Geffen School of Medicine in Los Angeles, California, USA. He is also Head of Outcomes Research in Hepatology at the Pfleger Liver Institute. Dr Saab received his BS, MD, and MPH from University of California Los Angeles (UCLA). He completed his residency in internal medicine at University of California at San Diego Medical Center and a fellowship in gastroenterology/hepatology at UCLA Center for Health Sciences. Dr Saab is board certified in gastroenterology and transplant hepatology. He has received honorary fellowships from the American Gastroenterology Association (AGAF), American College of Gastroenterology (FACG) and the American Association for the Study of Liver Diseases (FAASLD). Relevant publications Saab S, Hunt D, Stone MA, McClune A, Tong MJ. Timing of Hepatitis C Antiviral Therapy Pre and Post Liver Transplantation: A Decision Analysis Model. Liver Transpl 2010: 16: 748-59. With accompanying editorial. Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, Venick RS, Feist S, Goldstein L, Saab S, Hiatt JR, Busuttil RW. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010; 252: 652-61 Saab S, McTigue M, Finn R, Busuttil RW. Sorafenib as adjuvant therapy for high risk Hepatocellular Carcinoma in Liver Transplant Recipients: Feasibility and Efficacy. Exp Clinl Transplant 2010; 8: 307-13. Saab S, Bownick H, Ayoub N, Younossi Z, Durazo F, Han SH, Farmer D, Hong J, Busuttil RW. Differences in Health Related Quality of Life Scores after Orthotopic Liver Transplant with Respect to Selected Socioeconomic Factors. Liver Transpl 2011;17:580-90. Chak E, Talal AH, Sherman KE, Schiff ER, Saab S. Hepatitis C Virus Infection in the United States: An Estimated of the True Prevalence. Liv Intern 2011; 31: 1090-101. Wertheim J, Kupiec-Weglinski J, Petrowsky H, Saab S, Busuttil, RW. Major challenges limiting liver transplantation in the United States. Am J Transplant 2011; 11: 1773-84. Hong JC, Jones CM, Duffy JP, Petrowsky H, Farmer DG, French S, Finn R, Durazo FA, Saab S, Tong MJ, Hiatt JR, Busuttil RW. Comparative analysis of resection and liver transplantation for intrahepatic and hilar cholangiocarcinoma: a 24-year experience in a single center. Arch Surg 2011; 146: 683-9. Everson GT, Terrault NA, Lok AS, Rodrigo DR, Brown RS Jr, Saab S, Shiffman ML, Al-Osaimi AM, Kulik LM, Gillespie BW, Everhart JE; and the A2ALL Study Group. A Randomized Controlled Trial of Pretransplant Antiviral Therapy to Prevent Recurrence of Hepatitis C after Liver Transplantation. Hepatology 2013; 57: 1752-62. Rubin J, Ayoub N, Kaldas F, Saab S. Management of Recurrent Hepatocellular Carcinoma in Liver Transplant Recipients: A Systematic Review. Exp Clinl Transplant 2012; 10(6):531-43. Sood A, Cox GA, McWilliams JP, Wang HL, Saab S. Patients with Nodular Regenerative Hyperplasia Should be Considered for Hepatocellular Carcinoma Screening. Hepatology Research 2014; 44: 689-93. Matsuda T, Tonnu-Mihara I, Yuan Y, Hines P, Saab S, Italien GJ, McCombs J. External validation of the risk-prediction model for hepatocellular carcinoma [hcc] from the reveal HCV study. Value in Health. 2013; 16: A12. Campsen J, Zimmerman M, Trotter J, Hong J, Freise C, Brown R, Cameron A, Ghobrial M, Kam I, Busuttil R, Saab S, Holt C, Emond J, Stiles J, Lukose T, Chang M, Klintmalm G. Liver transplantation for hepatitis B liver disease and concomitant hepatocellular carcinoma in the United States with hepatitis B immunoglobulin and nucleoside/nucleotide analogues. Liver Transpl 2013; 19: 1020-9. Agopian VG, Petrowsky H, Kaldas FM, Zarrinpar A, Farmer DG, Yersiz H, Holt Cm Harlander-Locke M, Hon JC, Rana AR, Venick R, McDiarmid SV, Goldstein LI, Durazo F, Saab S, Han S, Xia V, Hiatt JR, Busuttil RW. The Evolution of Liver Transplantation During 3 Decades. Analysis of 5347 Consecutive Liver Transplants at a Single Center. Annals of Surgery 2013; 258: 409-21. Saab S, Manne V Akhtar E. Cirrhosis Regression in Hepatitis C Patients with Sustained Virologic Response after Anti-Viral therapy: A Meta-analysis. Liver International 2015; 35: 30-36. Saab S, Manne V, Bui V, Sundaram. Cumulative Radiation Exposure in Liver Transplant Candidates and Patients Transplanted with Hepatocellular Carcinoma. J Liv Dis Transplant 2014; 3 (1). Stepanova M, Wai H, Saab S, Mishra A, Venkatesan C, Younossi ZM. The Portrait of an Adult Liver Transplant Recipient in the United States From 1987 to 2013. JAMA Intern Med 2014; 174: 1407-9. Stepanova M, Wai H, Saab S, Mishra A, Venkatesan C, Younossi Z. The outcomes of adult liver transplants in the united states from 1987 to 2013. Liver Int 2015; 358: 2036-41. Al-hamoudi W, Elsiesy H, Bendahmash A, Al-masri N, Ali S, Allam N, Al Sofayan M, Al Bahili H, Al Sebayel, Dieter Broering M, Saab S, Abaalkhail F. Liver transplantation for hepatitis B virus: Decreasing indication and changing trends. W J Gastroenterol 2015; 21: 8140-7. Saab S, Jimenez M, Fong T, Wu C, El Kabany M, Tong MJ. Timing of Antiviral Therapy in Liver Transplant Candidates listed for Hepatitis C and Hepatocellular Carcinoma. Exp Clin Transpl 2016; 14: 66-71. Al-Hamoudi W, Elsiesy H, Bendahmash A, Al-Masri N, Ali S, Allam N, Al Sofayan M, Al Bahili H, Al Sebayel M, Broering D, Saab S, Abaalkhail F. Liver transplantation for hepatitis B virus: Decreasing indication and changing trends. World J Gastroenterol. 2015; 21:8140-7 Kuei A, Saab S, Cho SK, Kee ST, Lee EW. Effects of Yttrium-90 selective internal radiation therapy on non-conventional liver tumors. World J Gastroenterol. 2015;21:8271-83. Nguyen K, Jimenez M, Moghadam N, Wu C, Farid A, Grotts J, Elashoff D, Choi G, Durazo FA, El-Kabany MM, Han SHB, Saab S. Decrease of Alpha-Fetoprotein in Patients with Cirrhosis Treated with Direct Acting Agents. J Clin Transl Hepatol 2017; 5(1): 43-49. Ahmed A, Gonzalez SA, Cholankeril G, Perumpail RB, McGinnis J, Saab S, Beckerman R, Younossi ZM. Treatment of Patients Waitlisted for Liver Transplant with an All-Oral DAAs is a Cost-Effective Treatment Strategy in the United States. Hepatology 2017; 66(1): 46-56.
Eisai and Exegesis
Other programmes of interest
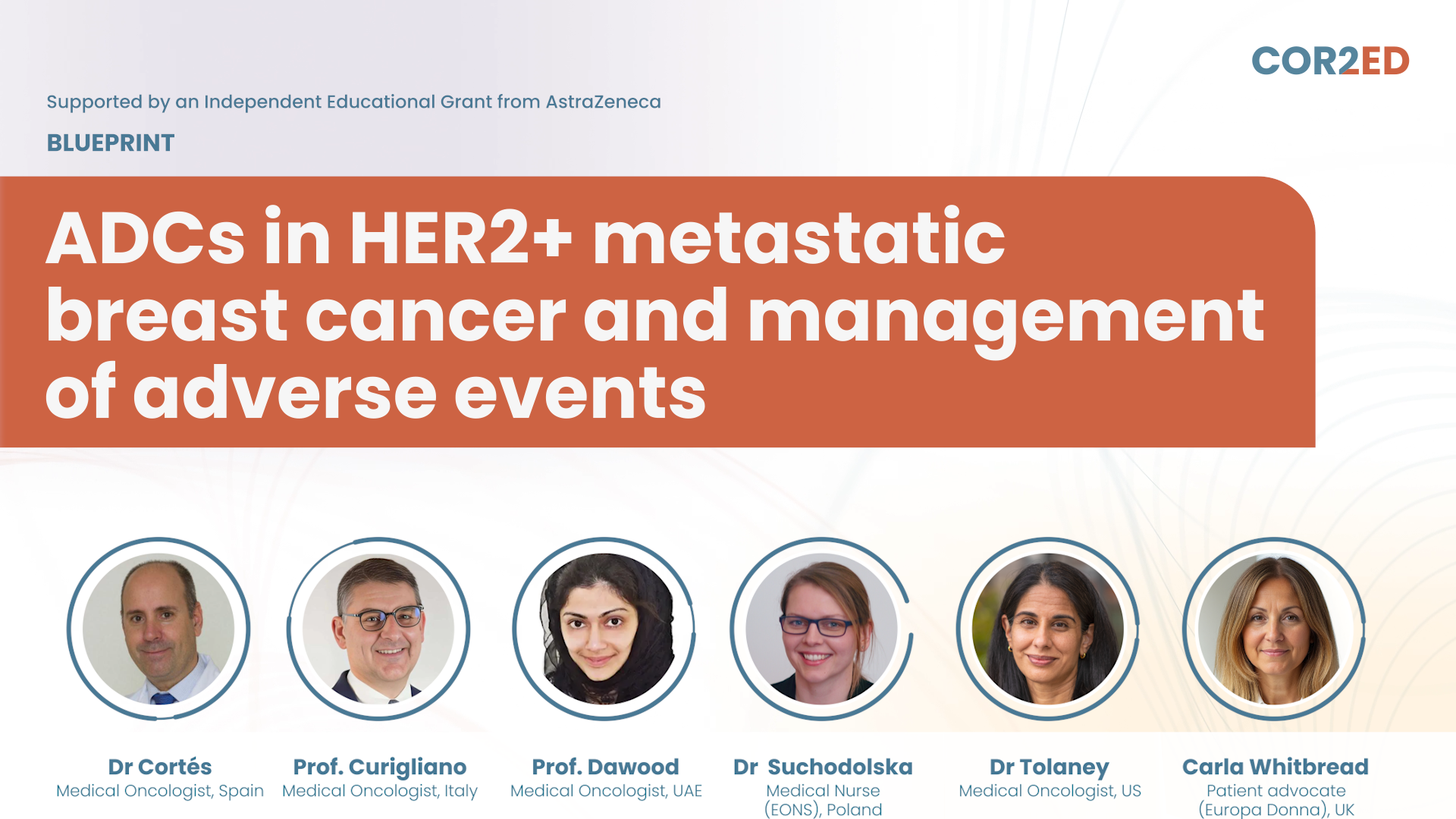
ADCs in HER2+ metastatic breast cancer and management of adverse events
Consensus-based guidance for clinicians and patients
Metastatic breast cancer: Understanding HER2-low and HER2-ultralow classification
A novel therapeutic framework
Experts
Dr Komal Jhaveri, Oncology Brothers (Moderators)Thriving beyond an EP-NEC diagnosis
Perspectives on treatment and care
Navigating extrapulmonary neuroendocrine carcinoma (EP-NEC)
Insights for patients and care partners
ESMO 2025: Gastric and gastroesophageal cancer insights for clinical practice
On-demand materials from an Experts Knowledge Share event



 Downloadable
Downloadable  20 MIN
20 MIN
 Feb 2026
Feb 2026