Rohit Gosain
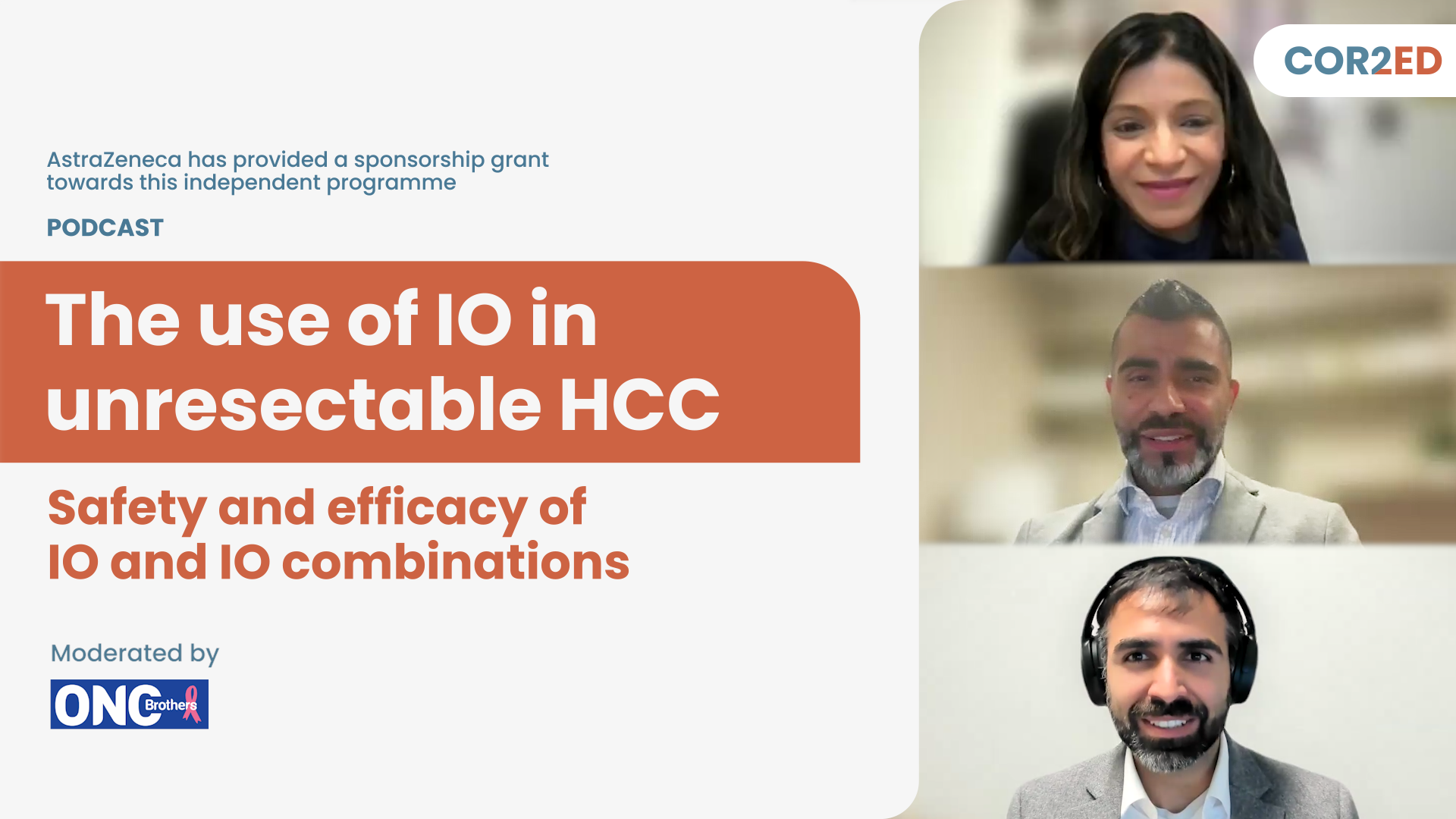
Hello and welcome back to the Oncology Brothers podcast. I'm Rohit Gosain and I'm here with my brother and co-host Rahul Gosain. Today we are wrapping out our four-part series on hepatocellular carcinoma. With a focus today on intermediate hepatocellular carcinoma, with evolving role of immunotherapy and stressing the importance of multimodality approach. Prior to this, in the past three episodes we have focused on advanced disease and treatment in frontline and on progression. And we've also covered intermediate HCC from staging standpoint. With that theme in mind, I'm joined by Dr Nina Sanford, a Radiation Oncologist from UT Southwestern. Dr Edward Kim, an Interventional Radiologist from Mount Sinai, New York and Dr Mark Yarchoan, a Medical Oncologist from Johns Hopkins. Nina, Ed, Mark, welcome.
Rahul Gosain
Mark, can we start off here with a brief overview of intermediate HCC and broadly the current treatment landscape? We have covered this a little more in depth in our third episode, but if you can lay some foundation down.
Dr Mark Yarchoan
Absolutely. Intermediate stage HCC is a bit of a historical term. It was really defined in an era when we didn't have effective therapies for HCC. And at a very high level, it refers to patients who have HCC that is confined to the liver and these patients, at least in theory, may be candidates for some sort of loco-regional approach to their therapy that generally can only be offered to patients with liver confined HCC. I think in a contemporary era, we're increasingly recognising that this is a super heterogeneous group of patients. They are patients who really have a systemic process here, where the scans may only show lesions in the liver but really, even though there is a propensity for liver metastasis, this is a systemic process, and these patients tend to have more disease and be better candidates for systemic therapy. I think, on the other end of the spectrum, there's a group of patients with intermediate stage disease where the goal is really to cure them through down staging and transplant. And then somewhere in the middle there's a group of patients who have, I think even though they have multiple lesions in the liver, this is more of a local process than a systemic process. And, at least initially, the goal is loco-regional therapy.
Rohit Gosain
Thanks for laying that foundation where loco-regional therapies are extremely important. As a result, the need for multimodality approach here. Now we have the combinations of IO with loco-regional therapies and this need only gets more important.
Nina, first, we need more representation of radiation oncology for BCLC to have a truly multidisciplinary approach. Now, diving into the topic here, can you touch on some of the modalities available for radiation oncology in this space, please?
Dr Nina Sanford
Yes, I think I completely agree with Mark, with regards to defining intermediate risk and how historically, it's sort of fallen into three buckets sort of down staging for transplant, or the systemic with greater disease burden, and then in the middle, the sort of destination local therapy. I think the lines are blurring between the three, though, hence the need for combination therapies. But I think radiation has a role in all those three frames. We think down staging to transplant, then radiation could be used as either bridge or down staging, in this case for intermediate risk if they're initially above the Milan criteria, both in, you know, down staging. If we think, destination loco-therapy, historically it's been TACE and now TARE. I think radiation has a role as well for more well-defined, isolated tumours that are intermediate stage. And then the last is historically, patients who have been treated with systemic therapy. We think of that, really for patients with greater than 50% liver involvement. I think Dr Kim can maybe talk about combination TACE and immunotherapy studies, but there is emerging data on the combination of radiation and systemic therapy as well. I’d just like to quickly highlight two studies with that regard. Because there's not a lot of data for radiation in the setting. But one is NRG/RTOG 1112. This is not immunotherapy, it’s sorafenib, like a lot of the studies started earlier used sorafenib, instead of more current treatment regimens. But this was a study randomising patients, with intermediate stage B or stage C HCC, though the majority were stage C. They were randomised to sorafenib with or without SBRT. And the study found that the addition of SBRT improved PFS from about 5 to 9 months, but also improved OS from 12 to 15 months. So I think, of course, the major caveat is that sorafenib is the comparison arm. But I think those data compelling to take it to the next trial with immunotherapy.
Also a smaller, retrospective study that was recently published in JAMA Oncology (Chiang et al., 2024). This was a study looking at combination of immunotherapy and SBRT in all patients, though about two-thirds of them or three-quarters, also got TACE as well. And complete response rates for these pretty extensive tumours, I think the median size is like 10 cm, the majority had vascular invasion was actually close to 50%. And I think that is compelling data, but still, you know, single institution, non-randomised. So I think going forward, we need more randomised data looking at radiation.
Rahul Gosain
That's great. Thanks for touching on this, because as a community oncologist, it is so important for me to partner up with my neighbouring Radiation Oncologist. And let's pass the baton on to Interventional Radiologist here. Ed, as an Interventional Radiologist, what are your thoughts on the data that we have in hand, be it for EMERALD-1, where we have durvalumab with or without bevacizumab with TACE and LEAP-012 with pembrolizumab and lenvatinib with TACE. Your thoughts around this and TACE versus TARE?
Dr Edward Kim
I think that both of those trials were read out as positive, with the primary endpoint being progression-free survival, and they're roughly similar, around 15 months. The difference, I think, in trial design between the two is that EMERALD-1 was really successive therapies. You do the TACE first and then you add really the bevacizumab, you start with the durvalumab. And that showed a benefit in terms of the primary endpoint. And then LEAP-012 was concurrent therapies. So really started at the same time with their regimen. And so, you have kind of, the same types of outcomes. You do subset analysis, higher disease burden, whether it's up to beyond seven or beyond six, all seem to benefit because you have multifocality of disease where transarterial therapies seem to derive a benefit. We have to see, right? Because in light of IMbrave050, where everyone is very excited about a positive primary endpoint of PFS. Ultimately, the median OS showed no benefit and everything else actually was statistically insignificant. And I think we have to really focus on these studies and look at the overarching theme. There may be trends that we see, but ultimately, if it's statistically insignificant and it's a negative endpoint, is there a benefit?
I think most people are kind of a wait and see approach with both EMERALD-1 and LEAP-012, looking at how is the median OS going to read out? Not to mention the heterogeneity of the intermediate stage. If we're using, let's say the, the Barcelona criteria, touching on the different therapies, I think downstaging, we know with established evidence, multicentre, prospective Phase 2 type studies (LEGACY study) that radioembolization really achieves that quicker and has a sustained response, with a duration of response that's quite long, up to two years, with our study, the RASER study. And so that is a, I think, different type of goal and patient population as opposed to the let's say, infiltrated. We have high alpha-fetoprotein (AFP) and aggressive tumour biology where, I think it's well-established that we go to systemic in those individuals. Now does LEAP-012 and EMERALD-1 bring into that type of patient population transarterial based therapy? It's yet to be seen. I think that is why there is the importance of multidisciplinary teams. And then, as Mark had mentioned, the multifocal disease without too much disease burden, whether you go by the Bolondi or Kinki criteria, then everyone has their own criteria, Japanese TACE criteria, etc. We're really looking at lower tumour burden, but in actuality we're trying to discern which patients may be having a less aggressive tumour biology that is contained within the liver, that is not potentially going extra hepatic, etc., with an aggressive tumour biology. I think that is a, crude measure based on tumour burden, how many nodules there are, in terms of, lower kind of aggressive tumour biology. Well differentiate HCC that could potentially derive a benefit from loco-regional therapy alone, TACE or TARE, etc. And then holding off on systemic therapy because I'm sure we can get into this discussion as well. But, how does combining therapy earlier on in the intermediate stage affect the data that we have with HIMALAYA, with IMbrave150, with nivolumab + ipilimumab, in the advanced stage? And so I think that is what people are trying to, kind of, elucidate right now.
Dr Nina Sanford
I wanted to quickly give my thoughts on EMERALD-1 and LEAP-012. I think this goes back to what Mark had mentioned. To me, they're really trials of whether or not to give immunotherapy upfront or later. Right? Like Mark mentioned, a lot of these patients are going to need systemic therapy later. Because unfortunately they're going to have progression. The criteria for LEAP, this is incurable cancer, that’s literally on the slide. So I think to call these trials positive, they really need to show an overall survival benefit. They're positive because the primary end point is PFS. But in terms of impacting patient care, we really need to show an overall survival benefit. In LEAP-012, the incidence of grade 3 to 5 adverse events with around 70% for patients in the combination arm, more than double with the TACE only arm. So it's a very costly drug. And you don't show a survival benefit. If you look at the curves that have been presented, I cannot imagine that long term you're going to see a survival difference. If you look at the curves presented thus far. Finally, I think there is some data showing correlation between PFS and overall survival for advanced HCC. But that has not been shown to my knowledge for intermediate stage HCC.
Rohit Gosain
Mark, I'm sure you got some interesting thoughts from medical oncology standpoint because again, we have been relying on the PFS quite a bit and that has been the debate. A lot of the trials, especially when the readout for overall survival is way down the road, how do you interpret the PFS aspect to it? But at least for HCC, things sort of move fast. So yes, I’d like you get your thoughts here.
Dr Mark Yarchoan
I don't disagree with anything that's been said. And I might say the same thing, but with a slightly different take. In the end, you know, I think there's been this natural creep of systemic therapy earlier and earlier in the treatment of HCC. And, you know, just for some historical context, when I was first treating this disease, a lot of patients would get repeated TACE or TARE or other loco-regional procedures to the liver. And eventually they would either run out of liver reserve because of repeated loco-regional procedures, or would just develop loss of tumour control. And by the time that they would come to see me in medical oncology, essentially, I would be having a hospice discussion with them. And that was actually okay because it wasn't like these patients were missing the opportunity for a great systemic therapy. We didn't have much to offer them. I think in the contemporary era where we have much better systemic therapy, what we really don't want is for patients to truly miss the opportunity to go on, potentially multiple lines of systemic therapy. So I think there is some natural creep as we get better systemic therapies, we want to move them earlier. And, there is retrospective data, at least with a propensity matching study (Kudo et al., Cancers, 2019) that for patients with larger tumour burdens beyond up to seven criteria, the sum of the diameter of the lesions, they may do better with upfront systemic therapy, than TACE at least, and that benefit, that overall survival benefit retrospectively, is actually driven by preservation of liver function. When we look at the LEAP-012 data and the EMERALD-1 data, it's very early data. I personally don't think that, at this point, it's truly practice changing. All we know is that the scans look prettier when you combine both modalities versus one modality. But I do think that it, sort of supports the general natural trend that's been happening anyway, that systemic therapy has moved earlier. And really, the hope is that if we can move systemic therapy earlier, number one, we don't miss opportunities for patients to get systemic control. But number two, we can really focus, loco-regional therapy on treating oligoprogression or residual lesions or debulking in the setting of systemic control, rather than just using systemic therapy as a last resort.
So, again, I think we need longer term overall survival data. The LEAP-012 study, at least overall survival is trending in the right direction, but certainly not at the point of statistical significance right now. So I think these data are eagerly awaited. I do think it will be very helpful to also have studies of systemic versus TACE in the intermediate stage, in like the REPLACE study and ABC study, because, right now it's all about combination and the sequencing is still a real question.
Rahul Gosain
Mark, can I push a little further on the LEAP-012 and EMERALD-1 data, based on PFS while we're waiting on OS. Have you adopted this already in your clinical practice outside clinical trials?
Dr Mark Yarchoan
Well, it's a very straightforward question, but I'm going to give you a sort of roundabout answer. I think my suspicion is everybody on this call has been combining systemic therapy and local therapy in the intermediate stage for much, much before these studies were ever published. In fact, every single major 1st line systemic therapy study includes intermediate patients. And there's a survival benefit to systemic therapy in that setting. So, I think some of this was happening naturally. I haven't done it more since the studies came out, because I think that the data is very preliminary. And I think, you know, I still think at this point these patients really should have multidisciplinary input come through an MDC, and there is really a lot of value to, institutional experience right now because I think the clinical data are still very challenging to interpret in these large studies.
Rohit Gosain
Mark, how does that tumour board conversation look like in your space? Or what is, rather, an ideal patient where you will utilise this approach? And then we'll ask Nina and Ed, on how their multidisciplinary approach works where medical oncologists have added some of the systemic therapy in upfront settings and you have rather seen some responsiveness here.
Dr Mark Yarchoan
Yes. I think it's hard to sum up, everything that we do in just a quick sound bite here, but I think that there are patients who benefit from systemic therapy. These are patients with larger tumour burdens, infiltrated disease, patients where there really is a good shot of down staging and systemic therapy can help achieve that goal. I also think there are patients who benefit from loco-regional therapy, and Ed and Nina can better define who those patients are. In my mind, patients come through the multidisciplinary care (MDC) and we go through two separate algorithms, and there are patients who may benefit from both. And, until we have longer term follow up, I think it's a case-by-case situation where we really think about these patients holistically.
Rahul Gosain
Ed, what is this conversation on your end at the tumour board?
Dr Edward Kim
I think the multidisciplinary tumour board, and we have also multidisciplinary office hours in conjunction with our transplant and our medical oncologists are across the street. I think it’s essential for taking care of HCC patients. As Mark was talking about previously, we know that, back when we had no options other than sorafenib, which was quite poor with the 2.7-month median OS benefit with the SHARP trial, it's not much. I would be at tumour boards where I say, all right, I don't think we can do any further loco-regional therapy for this, or it's not a great candidate. And my colleagues would say we have no other option, and kind of push us to do it. I think we are still undergoing a cultural shift now because the positive trials with systemic therapy are coming fast and furious, like literally every year. And so it's quite exciting. But I don't know if the medical community as a whole has caught up. And so we have to change that cultural mindset, for instance, where interventional radiologists are continuing potentially to do, transarterial based or loco-regional therapies over and over and over again to the detriment of underlying liver function. And so I think we need to educate better. In our tumour board, if I feel that we've exhausted loco-regional therapy, in the sense that the patient still has good underlying liver function, I will say, listen, why don't we hand off this patient? I'll give you an example. We do, let's say a Y-90 for a patient. And on follow up, there are multiple new lesions that pop up. Could I go after those lesions? I could, but there's probably something else going on. And we'll hand off to systemic therapy and say, hey, is there anything you guys can do and say, okay, let's try this. And if they progress after this and there's still Child-Pugh A, ECOG performance of 0, then okay, let's revisit loco-regional therapy. But they may be part of that 33% that has an objective response rate to the systemic, to the checkpoint inhibitor. Really if they do, it's fantastic. We know that they have a meaningful median OS benefit now of 17, 19 months for the advanced stage. This is very complex decision making and discussion, but essential to take care of HCC patients.
Rahul Gosain
Nina, anything to add here from a multidisciplinary tumour board discussion?
Dr Nina Sanford
Yes, I completely agree. I think there have been so many times where because in HCC there's so many treatment modalities, so many local treatment modalities, you think that one makes sense. And then someone says something, you're like, I didn't even think of that. But that's probably a better option. And I think for those of us who are focused on the local treatment, it's really important to know the other local treatments, like I've recently spent a lot of time learning the IR literature. I’m learning the surgery literature to really, see, you know, in a patient who could potentially qualify for several, what is the best one. Yes, I think the potential transplant is what really complicates things and can sometimes complicate the decision for local therapy, because a lot of times you're thinking, well, maybe I wouldn't give this patient local therapy, but that might be their only route to potentially qualify for transplant that could potentially compromise liver function. But, should you really give them that last opportunity to potentially receive curative treatment. So I think that is definitely a scenario that especially needs multidisciplinary discussion. But otherwise, yes, I totally agree with, what everyone else said.
Dr Mark Yarchoan
One more point, Ed spoke a lot about, the sort of earlier handoffs to medical oncology, but I think it's important to emphasise bidirectional handoffs because, you know, we're not curing that many people with systemic therapy. There are the occasional CRs. But, you know, I think we get a long period in some patients of excellent disease control and good tolerability of therapy and preservation of liver function. Eventually in most cases there's progression. Often that progression happens not uniformly but often in the liver, which is a more immune tolerant organ. And so, more and more, I think we need to adopt a culture where patients can go back to loco-regional therapy. It's a much more back and forth. At least at the institution where I practice we have shared office hours, a shared clinic and, it's very common for patients to come through that clinic, not just once, but repeatedly at multiple stages of their care. So I just want to emphasise, I don't think loco-regional therapy is going away. I think that sequencing is changing.
Rahul Gosain
Before we close, I'll take some clinical takeaways from the discussion and any final thoughts for our listeners on intermediate HCC.
Dr Nina Sanford
One thing I didn't mention, I just wanted to put a plug in for an upcoming trial. Probably opening next year through NRG oncology (NRG-GI012). One of the cooperate groups. So this is a trial looking at, as I mentioned, immunotherapy plus or minus SBRT. So this is, randomised trial of atezolizumab + bevacizumab or STRIDE plus / minus SBRT. Right now it's just for Barcelona class, stage C, so, you know, the more advanced and what we had talked about given current standards of care, but I would predict if new data comes out, they may also include some stage B. So definitely keep an eye out for that study. I think it's, you know, would really help provide data for radiation in this setting. And encourage folks to enrol. Thanks.
Rahul Gosain
Mark, your final thoughts and key takeaways?
Dr Mark Yarchoan
It's a great time to be a medical oncologist because we actually have things we can do that meaningfully help patients with HCC. I think we have some intriguing early data about combination therapy that fits with a broader trend. But, longer term follow up is clearly needed.
Rahul Gosain
Ed, your key takeaways from today?
Dr Edward Kim
It's essential to work within a multidisciplinary team for just multiple levels. Patient care, the whole aspect of patients potentially going to a curative transplant. And again, working with our medical oncology colleagues to hand off patients and as Mark had mentioned, to receive patients back. We've had patients that have gone on several years of checkpoint inhibitors. But checkpoint inhibitors initially got them there and then they have breakthrough progression and we can perform loco-regional therapy and still keep them, maintain their performance status and their underlying liver function. And also, we're investigating all these combination therapies, whether in the intermediate stage or advanced. I mean, the ROWAN trial is a Phase 2 study combining radioembolization and durvalumab and bevacizumab. And then there's the EMERALD-Y90 that's combining radioembolization plus durvalumab and tremelimumab. So I think it's an exciting time. There's a lot of options for patients.
Rohit Gosain
So there are multiple exciting trials that are taking place. Only time will tell how the overall survival data plays out. Nina. Mark, Ed thanks so much for your valuable insights.
Multidisciplinary approach is an extremely important aspect of medical management especially when it comes to HCC, and these conversations continue to reiterate that. Thanks for joining us. For our listeners, let us go over a quick recap. Intermediate HCC is a heterogeneous group requiring multidisciplinary approach. Today, with Drs Nina Sanford, Ed Kim and Mark Yarchoan, we had a chance to discuss more of liver directed therapies along with immunotherapy. As we continue to see the data in this space with multiple combining regimens, that is durvalumab with bevacizumab or pembrolizumab with lenvatinib, only time will tell how this all plays out.
Rahul Gosain
This discussion concludes our four-part series on HCC. We had a chance to cover available treatment options for intermediate and advanced metastatic hepatocellular carcinoma. Make sure to check out our other three discussions in this series. Thank you for joining us. We are the Oncology Brothers.
Tonke de Jong (COR2ED)
If you enjoyed this podcast and want to find out more then please look for the "Oncology Medical Conversation Podcast" under the account of COR2ED Medical Education.
Also don’t forget to rate this podcast, subscribe to our channel and share it with your colleagues. Thank you for listening and see you next time. This podcast is an initiative of COR2ED and developed by HCC CONNECT, a group of international experts working in the field of oncology. The views expressed are the personal opinions of the experts and they do not necessarily represent the views of the experts' organisations, or the rest of the HCC CONNECT group. For expert disclosures on any conflict of interest please visit the COR2ED website.












 Downloadable
Downloadable  5 MIN
5 MIN
 Mar 2026
Mar 2026