The role of VEGFR-TKIs in the treatment of advanced RCC alone or in combination
Georg Hutterer: Okay, so hello everybody and welcome to this podcast on the role of VEGFR TKIs in the treatment of advanced kidney cancer alone or in combination. My name is Georg Hutterer I am a senior staff member at the Department of Urology of the Medical University of Gratz, and I am really delighted and honoured to be joined today by Thomas Powles, who is a Professor of Genitourinary Oncology, he's the director of the Bart’s Cancer Center one of the most advanced cancer centres in Europe and lead for a solid tumour research in London UK and without doubt, represents one of the most prolific and I would say, influential contemporary researchers worldwide regarding advanced and metastatic kidney cancer, so welcome Professor Powles.
Thomas Powles: Well, thank you for that extraordinary introduction it's very sweet of you, some of it's true, I think.
Georg Hutterer: I think all of it. Now Thomas the landscape of the various approved medical treatment modalities for advanced and metastatic RCC changed dramatically let's say over the last 15 years. Providing impressive survival benefits, particularly, but not only in the clear cell renal carcinoma and there have been a number of important phase two and three studies over the past couple of years, involving tyrosine kinase inhibitors, especially in combination with the new immunotherapies, and this is reflected in the recent guideline
updates. Now you have a key involvement in various of these updates, for example, you're the first author of the brand new I would say update of the ESMO clinical practice guidelines from September, you’re as well co-author of the recent EAU renal cell carcinoma treatment recommendations from the European Association of Urology published at the end of May by Professor Bedke. Maybe you could give us an overview or take us through the recommended systemic therapies for patients with advanced renal cell carcinoma.
Thomas Powles: Yeah, thank you Georg. So I think that there's been a seismic change in the last five years and we've moved now from frontline VEGF targeted therapy, which was sunitib or pazopanib, to frontline PD-1 inhibition based therapy, which has been with nivolumab or pembrolizumab and the question is what second drug do you add to these.
And there are two current approaches, one is to add a CTLA-4 inhibitor, the first trial was Checkmate 214 ipilimumab and nivolumab and we've just seen the five-year update of that data with a hazard ratio of 0.68 in the intermediate and poorest population, that data looks terrific. And then the second approach is to add in a VEGF TKI and there are three combinations there, Keynote 426, that is the axi pembro trial that showed a higher response rate, a longer PFS but also initially a hazard ratio 0.53 for survival, that is now currently 0.73 at the most recent update. And so that established axi pembro in good intermediate and poor risk patients. The next trial that came out was Checkmate 9ER and that looked at cabo nivo the survival signal of that looks very similar.
And then the final trial is the CLEAR trial of lenvatinib and pembrolizumab and that came out most recently, hazard ratio for PFS 0.39, 73% response rate data looks great has ratio for survival also statistically significant and so that has joined axi pembro and cabo nivo as an option for good, intermediate and poor risk patients.
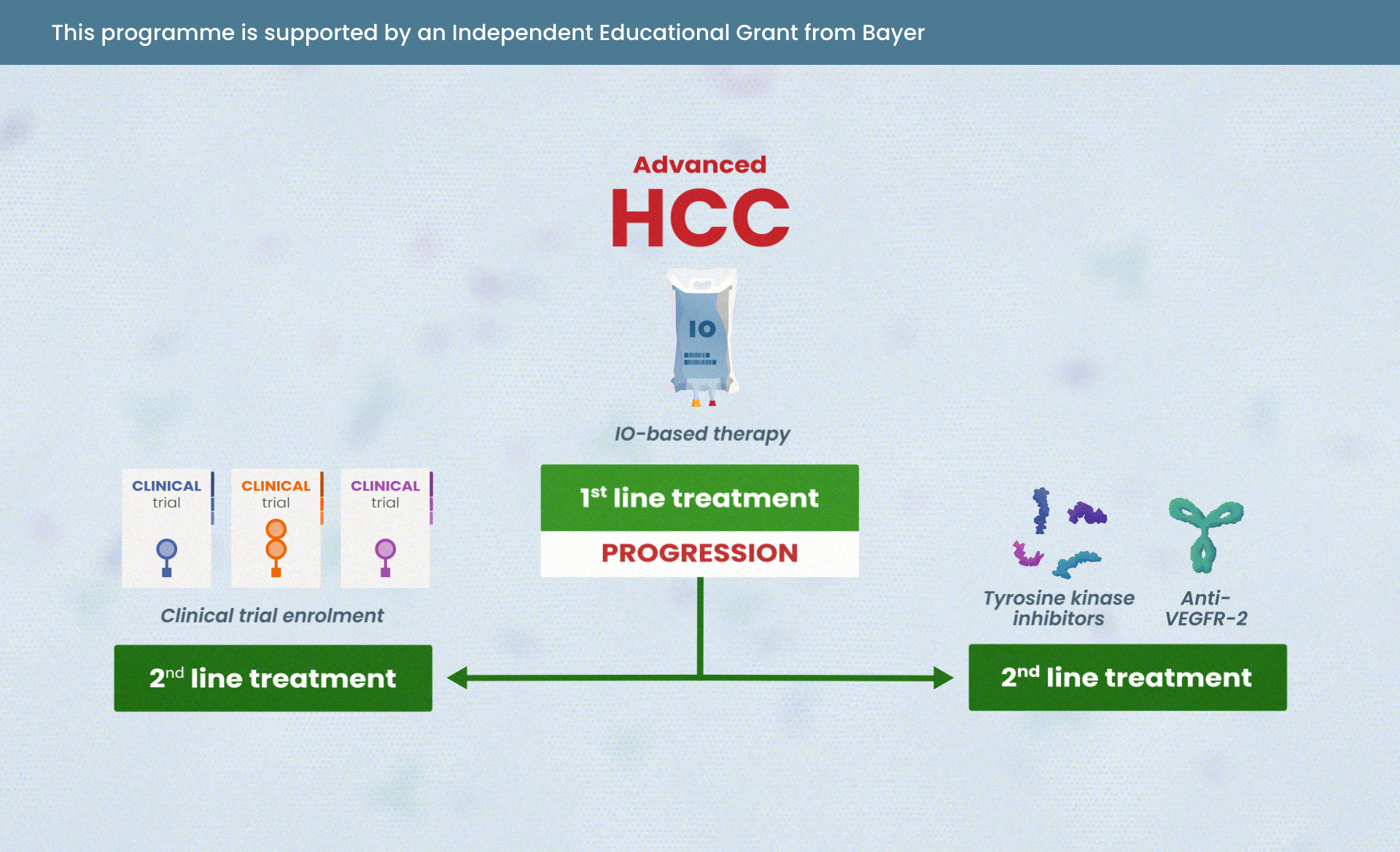
So good, intermediate and poor, any of the VEGFR TKIs. Intermediate and poor ipi nivo. At progression we don't have much data, because all the frontline trials have changed everything. So, we've got a series of single arm relatively small trials looking at cabo, axitinib, pazopanib and there’s some retrospective data on tivozanib out of Tivo-3. And all of those drugs look to have response rate of about 20%, this is much weaker evidence, it's Level 3B as opposed to level 1A evidence.
So, the reality is we've got ongoing randomized trials in this space, now we just trying to address these questions. Sequencing drugs is still important but getting PD-1 based therapy upfront is also really important.
Georg Hutterer: So, great thanks for this overview, Thomas and now may I ask you which approach do you use personally.
Thomas Powles: Well, you know I think my message to people is that I don't mind which of those regimes people use but do learn how to do it and choose one and do it well because it's more challenging than sunitinib and pazopanib to give combination therapy; either ipi-nivo or VEGTKI-IO therapy and there's more toxicity, there's more complexity, there's issues around which drug to discontinue how long to continue for, sunitinib and pazopanib were quite straightforward when patients got into trouble they stopped the drug, and they got better. That's not the case with these new drugs.
With ipi-nivo the combination period during the first 12 to 16 weeks is quite challenging.
The patient is likely to develop toxicity and that requires careful management, using a multidisciplinary approach. The attractive components of ipi-nivo is after those first 16 weeks patients are essentially on nivolumab monotherapy, which is actually well tolerated, on top of that, ipi-nivo has the longest follow up data and has maintained its overall survival signal. The VEGF-TKI- immune combinations and Len-pemb, Cabo-nivo, axi-pembro all show very similar things. They show higher response rates, really good disease control, ipi-nivo doesn't have as good a response rate, or as good disease control. They show great tumour shrinkage, and they show great progression free survival. They are probably easier to give during the first 12 weeks because you could just stop the VEGF-TKI and for many patients the toxicity gets a bit better sometimes yes with colitis you've got to get steroids, with pneumonitis you have to give steroids but it's a bit, it's honestly it's a bit easier. On top of that we don't yet know whether we're going to maintain those OS signals that ipi-nivo seems to be doing. There is some data to suggest that ipi is good for longer term outcomes, we don't know that yet, but this is a this is a field that's evolving. So, you asked me a direct question which do I use. And my direct reply to that is I would rather we'd learnt more about how to give the drugs than picked one that we think is best.
If you look at the data sets that are in front of us, for the VEGF-TKI-immune combinations the hazard ratio and the response rates for PFS for lenvatinib-pembrolizumab look really impressive. They've got a 0.39 PFS and they've got a response rate in the 70%’s, their data points look great.
For the cabo-nivo data, the quality of life, data looks really attractive the cabo’s given at 40 milligrams I can see that being attracted for some people. I can see other people saying you know cabo’s a great drug nivo’s a great drug, I want to give those two together, so I can see that being attractive. And then for axi-pembro the first combination to come out, it's got the longest follow up, axitinib it is probably the easiest of all the VEGF-TKIs to give, it has a short half-life.
Making that really important management toxicity, in my perspective probably the easiest, so I can see why that's attractive as well as I said before, pick one and use it well.
Georg Hutterer: Okay, thanks, a lot for the good answer I mean so would you maybe this is a provocative question but we know Tony Choueiri from Boston Harvard I think he gave a very well lecture at the ESMO now, in September at the virtual where he's talking about optimizing the first line treatment in metastatic clear cell RCC and would you agree with him in his last slide I remember talking about systemic therapy, where he said, theoretically, if you don't have a very rapid progression no need for immediate response he will either go for nivo-ipi versus IO plus VEGF TKI if you need a fast response, maybe if the candidate is not ideal for immunotherapy like <<inaudible>> diseases if tumour burden is very high.
Thomas Powles: yeah, so I think that's a good question, I mean clearly it's become quite complicated because you can't give ipi-nivo to the good risk patients it's not licensed in that indication and many patients with slower growing tumours have good risk disease, so you can't really give ipi-nivo to that group of patients.
I think one of the issues is I’m not sure the IMDC classification for good, intermediate and poor risk is a good molecular classification it doesn't tell us which tumours are biologically going to respond to immune therapy, it's a classification based on risk factors, which are clinical risk factors. We have developed new molecular biomarkers we're developing them, Brian Rini and Bob Motzer had a cancer cell paper recently defining seven molecular classifications for renal cancer and two of those are immunogenic and three of them are VEGF targeted.
And it may be actually that it's better to do a molecular analysis, rather than the IMDC classification, to work out which patients need immune combination therapies, but more importantly, which need that that VEGF backbone. Because for some patients, if you give ipi-nivo unfortunately the cancer progresses through and that's a real problem for a significant group of patients. And so Tony's right, because what he's saying is, if you give more indolent tumors ipi-nivo most of those you could then rescue with VEGF targeted therapy if you want to, but the challenge with, that is, many of those patients will be good risk disease and you can't give it to them anyway. So, I agree with Tony, but I think the solution to this ultimately would be to move to better biomarkers.
Georg Hutterer: Another question just because also Tony Choueiri mentioned what about adjuvant immunotherapy becomes sometimes a reality which it seems also a matter of time. I guess the treatment in the first line will even get more complicated than it already is, you would agree with that?
Thomas Powles: Yes, it will complicate the issue. And maybe the most important question there Georg is what happens if patients progressed soon after or on immune therapy, should they be treated with more immune therapy or should they get single agent VEGF TKI therapy and I guess one of my questions to you was are you still in your practice, is single agent VEGF TKI therapy, is that something that you're still using widely.
Georg Hutterer: Not in the first line not, no, I mean we stick to the to the combinations and first line if the patient is eligible, we especially here by I think it's the general way in Austria, we have like tumour boards once a week with the Department of oncology so I would never, for example, switch treatment alone without talking to an experienced oncologist at the setting.
Thomas Powles: With single agent VEGF TKI therapy we sort of, there is a debate in the IMDC good risk population, and that debate is gaining momentum. The reason why that's the case is in the forest plot analysis of the cabo-nivo, axi-pembro and len-pembro trials there's a clear survival benefit in the intermediate and poor risk patients, but in the good risk patients the confidence interval always crosses the one barrier.
Now, there were two reasons for that number one is it's an exploratory analysis of a subset that's underpowered. And because the patients have favourable risk disease there are relatively few events, so the confidence intervals, are wide nevertheless they are hovering around the one area, and some people say well, if they're hovering around the one area, why would you want to give combination therapy when you can give single agent therapy.
The ESMO and the EAU guidelines group both feel that, because the combination is associated with higher response rates and better PFS and the OS is still immature, we don't yet know that there isn't going to be a really big significant tail to that curve so as it's an exploratory analysis I think it's reasonable to give it the benefit of the doubt. But actually, as that changes if the data was to change with time and the meta-analysis becomes stronger, then perhaps people may go in a different direction.
Georg Hutterer: So, thanks now we've talked to you about the efficacy I mean another problem is there is no robust phase three data, how to move on in the second and higher lines, but I mean this is an old question. I would like to ask you is sticking to immunotherapy I mean the side effects sometimes require us to implement various dosing strategies can you maybe tell us which side effects, you were most concerned about, for your patients and how you manage them.
Thomas Powles: Yes, of course, and thank you, I think the first issue is, what do we do in in patients, whose cancers have progressed after VEGF TKI-immune therapies or immune-immune therapies and to answer your question directly I don't know, no one does we haven't done enough great trials, we’re doing those trials at the moment and we'll find out in two or three years’ time. As it currently stands, the ESMO and the EAU guidelines are aligned. And essentially, it's use a VEGF TKI that you've not used already.
Many people favour cabozantinib because that's a drug, which many people use. I'm very keen on axitinib also, but if I use axi-pembro front line which I quite like frontline, then why not give cabozantinib second line.
There's no evidence currently that adding an immune therapy on top of that is of any benefit. And in terms of the side effects, the side effects of this VEGF TKI you can expect to be similar as before. The one difference Georg which I think is really relevant is if you sequence the VEGF-TKI directly after the immune therapy, immune therapy has a longer half-life and you're likely to get more side effects at the beginning, because you and get the VEGF-TKI-immune combination. So let's say the patient's 12 weeks into ipi-nivo they progress in the liver and you want to give them a VEGF-TKI if you give them cabo like within a week they'll then be on cabo-ipi-nivo. Because ipi-nivo will still be in the system and that's associated with the transaminitis and is associated with other immune related toxicity so be really careful of that that's something which was caught out my group before.
Georg Hutterer: So, Thomas may ask you how are you managing the side effects if you still treat the patient with a single agent VEGFR-TKI because I mean we have much more, also in terms of years of treatment. Coming up like almost like over a decade right like with sunitinib or sorafenib so on and so forth experience is much longer than with the immunotherapy. So what are your thoughts about this?
Thomas Powles: So, my thoughts about the management of VEGF-TKI, single agent VEGF-TKI therapy is. I think at the moment, the really important thing is that you establish patients on the right dose of drug during the first four to six weeks.
I say to patients look you are going to start this drug we're going to start on this dose if you have side effects, or you don't like it miss a day here miss a day there wait till those low side effects go, give us a ring of course, but the reality is that what we're doing during the first part of this is we're giving everyone a high dose to start with and then we're going to see how you get on and it may well be that you end up on a lower dose so don't be surprised if you get side effects, obviously the classic side effects of hypertension and hand and foot syndrome, lethargy, diarrhoea, mucositis, they are pretty much for all of the VEGF-TKIs, some a bit higher some a bit lower, but in the grand scale of things, all are possible.
What I would say, from there is that once you're established on that dose and you're on chronic VEGF-TKI therapy it's really important that patients don't put up with bad toxicity.
Because some patients feel they have to just keep going on the cancer drug and they can't possibly miss it and actually there was a recent study called the STAR study which looked at intermittent sunitinib and actually it's probably okay to have significant treatment breaks if patients really need them, and so missing a week for a holiday or a family wedding or missing a few days here and there, stopping for diarrhoea, resetting the diarrhoea and restarting. All of these models are attractive and the same to some extent applies in combination therapy, the one difference in combination therapy with immune therapy is if you've got diarrhoea, for example, the patient develops diarrhoea you need to make sure that that's not purely immune related diarrhoea because patients will need steroids under those circumstances so it's reasonable with mild toxicity to stop the VEGF-TKI and see the adverse events go away, but if they don't go away or heaven forbid they get worse then you need to intervene with steroids and that's why it's much more complicated, giving the combination, rather than the monotherapy.
Georg Hutterer: Yeah, thanks Thomas for your insights and I think very interesting discussion, and maybe could I ask you to give just a short summary of what we talked about.
Thomas Powles: Georg and thank you for all the questions, I think that essentially can see, the important thing is, I think everyone now recognizes that kidney cancer, clear cell kidney cancer particularly, has changed, that PD-1 based therapy with either VEGF-TKIs or with a CTLA-4 inhibitor is now the standard frontline care.
I think we're showing long term durable benefits that we didn't see before, we're seeing longer progression-free survival, we're seeing much better results, the question is for me now can we in Europe translate those clinical trial results into real world data and make sure that we get these drugs into patient safely, as I said previously there’s serious toxicity issues that need to be addressed to maximize the outcome of the patients and the final bit is we're now developing triplets and I hope biomarkers which will continue this story, and perhaps improve outcomes further.
Georg Hutterer: So, thank you, thank you again for the great discussion was good talking to you and we'll say goodbye and have a nice day.
Thomas Powles: You as well Georg, lovely to see you, thanks for the questions.








 Downloadable
Downloadable  5 MIN
5 MIN
 Jun 2025
Jun 2025