In the third and final episode, Dr Jason Alcorn and Dr Alicia Morgans discuss adverse events associated with PARP inhibitors and the management of them, in particular thrombocytopenia, gastrointestinal effects and fatigue. Jason provides some insight into how nurses support and communicate with patients, the importance of early reporting of side effects and how to manage these. Finally, the ongoing trials of PARP inhibitors in combination with other prostate cancer treatments are also considered and what these trials may mean for patients.
Podcast Episode 3: PARP inhibitors in prostate cancer: Management of adverse events and the importance of communication with patients
Brought to you by:
Dr Jason Alcorn, Mid Yorkshire Hospitals NHS Trust, West Yorkshire, UK
Dr Alicia Morgans, Dana-Farber Cancer Institute, Boston, USA
Please note:
GU NURSES CONNECT podcasts are designed to be heard. If you are able, we encourage you to listen to the audio, which includes emotion and emphasis that is not so easily understood from the words on the page. Transcripts are edited for readability. Please check the corresponding audio before quoting in print.
This GU NURSES CONNECT programme is supported through an independent educational grant from AstraZeneca. GU NURSES CONNECT is an initiative of COR2ED
The views expressed within this podcast are the personal opinions of the authors. They do not necessarily represent the views of the author’s academic institution, or the rest of the GU NURSES CONNECT group.
Jason Alcorn: Hello and welcome to the third podcast in the series covering PARP inhibitors in prostate cancer. Today, we're going to be discussing management of adverse events and the importance of communication with patients. I am Dr Jason Alcorn and I'm a nurse consultant for Uro-Oncology and Andrology at the Mid Yorkshire Hospitals NHS Trust in the United Kingdom and a member of GU NURSES CONNECT. I'm delighted today to be joined by Dr Alicia Morgans. Welcome Alicia, perhaps you'd like to introduce yourself.
Alicia Morgans: Thank you so much, Jason. I'm a GU medical oncologist and the medical director of the survivorship programme at the Dana-Farber Cancer Institute in Boston in the US, and I am so delighted to be here with you today.
Jason Alcorn: So, Alicia before we delve into our discussion on adverse events associated with PARP inhibitors and the management of them, perhaps you could set the scene for our listeners with a brief introduction to PARP inhibitors in prostate cancer?
Alicia Morgans: Of course, so I think the field has really been transformed in the last few years because we have in the U.S. and in many other parts of the world two PARP inhibitors that have been approved for the treatment of advanced prostate cancer. These are specifically approved for patients who have DNA repair defect mutations, and those mutations can be either germline or somatic, which is important because about half of the mutations are going to be germline and about half are going to be somatic. This has already been discussed and really, I think, has been highlighted in terms of the importance of getting testing for both types of mutations. I'm really excited to understand how we can use these for our patients to really try to control the disease. And adverse event management is a huge part of that because the drugs only work if we can support our patients to receive them.
These two PARP inhibitors that are currently approved are olaparib and rucaparib, and they have slightly different approval indications. But there are others that are in late stages of development, including niraparib and talazoparib. So, I do think that this is an area where we're going to see a lot of development in the short future.
Jason Alcorn: Thanks, Alicia. So, starting to think about adverse event management, as we know, close collaboration between the physician, nurse and the patient is key to ensuring early reporting of the adverse events as well as ongoing management. Can you tell us how the physician and nurses’ partner effectively in the United States to manage these adverse events?
Alicia Morgans: I'm happy to, and as you mentioned, it really is a partnership and a team approach for all that we do for our patients with prostate cancer is a critical part of how we are able to really support the needs of our patients. From my perspective, from the physician’s perspective, I of course counsel the patient as I'm writing that prescription about what needs to happen in terms of monitoring and what the patient needs to look out for as he goes home and is using the treatment.
This setting the stage, I think, is so important because if someone knows what to expect, he can be on the lookout and can really intervene quickly when the first symptoms or concerns arise. Or he can communicate back with the clinic, which is something that often ends up going to our nurses. But that anticipation of what might be coming in the future, I think, really helps people to feel more comfortable.
I always have patients come back at about four weeks after they start the treatment with a PARP inhibitor because it's important to check a complete blood count and make sure that they aren't developing cytopenia’s.
Of course, as I mentioned, having the patient understand that he or his loved ones can reach out to our clinic and engage with me or with our nursing team to talk about whether they might be developing some fatigue or some GI upset is also important, and our nurses and our nurse practitioners and physicians assistants usually field those calls or messages through the electronic medical record to try to help patients think through whether they may want to ramp up the dose slowly over a few days, for example, if they have some GI distress, or if they're having a lot of fatigue to think about strategies to improve that with afternoon rest or even increasing exercise, which does help with fatigue.
And usually, it is the nursing team that ends up engaging with the patient between visits. Then, of course, as we go along, I continue to follow that complete blood count when I get those blood counts I also do check kidney function, liver function just to make sure that electrolytes are OK as well and ensure that the patient's on track.
So, Jason, I'm really interested to hear how this compares to how the nursing team and the physician team work together to help patients in the UK.
Jason Alcorn: Yeah. Alicia I think, it's very, from what you've described there it's very similar in that we tend to, nurses tend to be the first port of call or the buffer between the physician and the patient. And the main difference, I think, comes in that we actually undertake a lot of the monitoring so the physician would initiate treatment, and then we would pick up the monitoring and undergo that and undertake all the visits with the patient, so we become very involved with the patients.
Generally, we would only involve the physician if there were some issues that we couldn't manage, such as there was some GI issues that we weren’t managing very well or came outside of our remit and then we would need further expertise, input in that. And then we would get in touch with the decision to help with those issues.
And also, like the blood, as you indicated earlier, the blood work up appears to be at odds or there are some anomalies then we would involve the physician at that point. We try to have multiple communication routes because not every route is the same for every patient and every patient likes to communicate differently.
And I think you've touched on some of those areas there in that email, or with electronic records which are becoming more familiar in the UK now, and some of those have got communication routes within them and also the standard ones like we would telephone and email, but also patients, especially in the time we've been in will reach out to anyone who's listening. So even the family practitioners, we use their system so that they can send us messages that they may receive from patients. So, we try to cast the net as wide as possible so, it makes it easier for the patient to contact us and get that help and support that they need.
So now let's talk about the safety profiles of the currently approved PARP inhibitors, olaparib and rucaparib. These treatments have been used in other tumour types, such as ovarian and fallopian tube cancers for some time. So, in their arenas the safety profile is well established in that population, at least. But there's going to be some common side effects or adverse events within the prostate cancer trials that have undergone. And also, in the prostate cancer population. And what do you see that those potential adverse events are?
Alicia Morgans: Well, thank you for highlighting this. And like you said, it is good to know that PARP inhibitors are used in other disease settings so that we do have that information from other populations. What I think is interesting is that the side effects tend to be actually a little bit different, and some patients with prostate cancer may have maybe better tolerability than some of our patients with ovarian cancer, for example, who are also dealing with peritoneal spread of the cancer. And of course, that can contribute to some worse GI effects from the cancer itself, not necessarily directly and only related to the treatments. So, patients with prostate cancer may even have slightly better side effects in some areas as compared to some of those safety profiles for the other disease settings.
But generally, the way I think about it is that these are pretty well tolerated drugs. And that's important because as an oral option for our patients, that they really are seeking when it is available to them because of the convenience, it's nice to know that they're generally well tolerated, and their safety profile is also one that is usually pretty mild from my perspective, of course. But the adverse events are important in terms of making sure that we monitor for them because we need to identify them in order to ensure that we do support our patients and of course, keep them safe while they're taking these treatments.
The most common things that we see, as I mentioned before, are things like fatigue and sometimes some nausea or loss of appetite. But we also have to monitor for cytopenia’s, the development of things like anaemia and thrombocytopenia, can be relatively common, but again are usually on the milder side of things. So not necessarily things that we have to intervene on, but they are things that we do need to watch for. Some patients can also develop some diarrhoea, so these GI effects are things that we might expect again from an oral treatment that's directly engaging with the GI tract and then some headache as well.
But generally, as long as we educate our patients, as we're trying to start a medication, I think patients can really be on the lookout for the development of any side effects and can communicate early if they do develop them so that we can typically keep patients on treatment. And in the studies, there's a relatively low rate of discontinuation of treatment. And although sometimes there is a dose reduction, often if we do continue to monitor patients, we can bring back patients, bring them back up to normal levels as long as those adverse events do resolve and many of them do within the first six months of treatment, for example.
In terms of differences between the agents, I would say that they're actually quite similar and we do think of these effects as generally being class effects. So common ones that are common between the two are those cytopenia’s, anaemia, thrombocytopenia, sometimes lower levels of white blood cell counts but that's more rare, and fatigue and GI effects. And so, these are pretty common between the two. I don't necessarily choose between the two because of side effect profile, because they are so similar. Olaparib does have mentioned potentially thromboembolism or PE in their label, and both of them we need to think about long term development and monitoring blood counts because there is the rare potential for development of MDS or potentially a leukaemia.
So that's myelodysplastic syndrome, which can be characterised in a lot of ways, but usually is, low blood counts from bone marrow effects and again, is something that we'd want to monitor for and we can with our complete blood counts. And then usually I have not seen that in any of my patients in clinic, but with PARP inhibitors in general, that is something to think about.
Jason Alcorn: So, you mentioned studies earlier and we mentioned there's some drugs that are in late stages of development, such as niraparib and talazoparib. Do they appear to be any different to olaparib and rucaparib?
Alicia Morgans: Yeah. You know, they're actually, in many ways, very similar. Again, a lot of the complications that I mentioned are considered class effects. However, there was a slightly higher incidence of thrombocytopenia and hypertension associated with niraparib. So, things to think about. But these are things that we are monitoring for anyway, and I don't think should niraparib reach the point where it is approved, I don't think that this would necessarily preclude us from using the drug, just things for us to consider as we're trying to keep our patients safe and well on treatment.
Jason Alcorn: So, as you highlighted earlier, with these drugs and a lot of treatments for prostate cancer, that fatigue is a common side effect and that is something that often gets reported by the patients to the nurses, and especially because these patients will have had some form of hormonal treatment as well and we know that through the hormonal treatment, they can get side effects of fatigue, especially through things like weight gain and things like that. So, the fatigue side effect is going to be compounded by these new drugs then as well. So, we have to be mindful to educate our patients on that and that it may get worse. And I think it is important for the nurse, or the physician seeing the patient to probably get a baseline of what the fatigue is at present so we can monitor it going forward and in educating the patients would you agree that we look at, as you mentioned earlier, like the anaemia’s, the iron deficiency anaemia’s, or GI effects that can also impact onto the fatigue of patients? I know one of the things that we encourage patients is to undertake regular rest through the day, to plan the day so when they've got more energy then they can do things and at other times they can take that rest and not to be guilty because some patients feel guilty that they can't do things as they used to do, but also try and ensure they have a good sleep pattern as well. So, it is important that we keep patients active and we try to encourage them to exercise as much as possible, little and often and build that up, you know, through walks, or whatever helps them.
But also we can use technology. There's actually in the UK there’s a phone app called ’Untire’, which was developed by a former cancer patient who suffered with fatigue, which can help patients in managing the fatigue. Would you agree with that?
Alicia Morgans: I completely agree and thank you so much for sharing those approaches. I would say that I think it's important as we continue to monitor the complete blood counts over the course of especially the first year, I do keep an eye on them monthly and I try to understand all of the multifaceted components of what could be affecting the fatigue.
Certainly, low blood counts can do that and an understanding if a patient may be developing worsening anaemia, if that's related to the treatment or perhaps related to nutrient deficiencies like an iron deficiency, anaemia or B12 anaemia that we can intervene on is really important because understanding that gives us the opportunity, of course, to continue our treatment, but also improve the anaemia by really targeting the underlying problem. Of course, we want to understand if a patient had fatigue at the beginning and if most of the fatigue that's ongoing is related to the androgen deprivation therapy that the patients still on and use of apps, as you mentioned and planning the day so that patients can take a rest in the afternoon, if that's when they seem to get tired but be more active in the morning makes absolute sense and encouraging physical activity to really maintain physical function, even if that individual having fatigue, is a critical piece.
And finally, I would say that sleep issues are relatively common in men with prostate cancer not related to the disease, but just related to ageing. As many of our patients become older adults, they can develop insomnia for many reasons. One that is relatively easier to intervene upon is obstructive sleep apnoea, if we can diagnose that, it's not related to cancer and it certainly can be affected with interventions like CPAP machines and others, that can help patients reduce their fatigue and really have a better quality of life. So, understanding that underlying cause, digging into that, whether it's related to the treatment, to the cancer or to something else can be really helpful.
And then as you mentioned, GI issues like nausea and vomiting sometimes lead patients to feel they’re not well, they don't want to take their medication or they just generally feel like they're limited. When you see a patient who's developing GI issues, which is probably the other thing that I see more commonly at the start with PARP inhibitors, but of course resolves pretty early on as well, what do you do for those patients with GI issues, Jason?
Jason Alcorn: The first thing that I would do, I would ensure that at the start of the treatment that has been explained that we could get some of these issues and hopefully give him some advice at the start so the patient can self-manage as much as possible. But there probably would come a time when they're not able to do that and they’d get in touch with us, and we would provide some dietary advice look at what diet, what foods are they eating? Is there anything that they're eating that is bringing on these issues for them and then try and avoid those foods. And some of the common foods unfortunately for some patients, are the foods that they like to have most, such as chocolate, or alcohol or caffeine. And also, you know, for those patients that do like to smoke, then you know, these are going to cause them issues and we will give them advice to avoid these issues.
And if there were a time where they’re reporting some foods that are not able to take or they’re in extreme distress with it, we probably think to fetch in our colleagues from dietician services to try and help manage that as well, to give more specialist advice. If symptoms persisted, we could look to using things like anti-emetics. So, as you say, helps them take the medication, keeps them on the treatment much longer, or if it's other GI issues such as diarrhoea, we may look at using loperamide, but we try not to use them long-term so people are dependent on them so they don't know when the issues have stopped. And then if it continues for any length of time, then of course we would always speak to the physician and get their input into it, so we knew that what we're providing, what’s the best treatment and everybody knew what was going on with that patient.
Alicia Morgans: I completely agree with all of that and I think GI issues, although they can occur at the start, as I said before, they typically resolve within the first couple of months. And for most of my patients, if they have any GI concerns to start, if they just back off the dose a little bit and then titrate the dose up over about a week. These issues seem to resolve.
So, these are some of the issues that I find much easier to manage. And for anyone who's already kind of feeling a bit nauseous or has some GI issues in their past, I often will start them at that titration up over a week just to avoid any potential nausea that they may have or loss of appetite when they start, because we want to start them off as well as we can and ensure that they feel comfortable.
Jason Alcorn: Thank you Alicia. I know you've probably mentioned already, but just for our listeners, you know, is there any specific monitoring that we should perform when using PARP inhibitors?
Alicia Morgans: Absolutely. So, as I mentioned, measuring blood counts is an absolute must, and I always also include the differential just to make sure that I understand if there is a low white blood cell count, I know if the patient actually is developing neutropenia. That's relatively uncommon in my clinic, but it is something that I always watch out for because we certainly wouldn't want patients to be vulnerable to infection.
As I mentioned before, as I'm getting a blood count, I also always get a metabolic panel and I do a complete metabolic panel so that I can ensure that I have complete understanding of what's going on with hepatic function as well as kidney function, and I have all of the electrolytes there as well.
We also recommend blood pressure monitoring, and this is something that we do in clinic, as all of our patients come in, we always get a blood pressure as well as pulse, you know, their vital signs. And this is going to be, I think, especially important as niraparib comes into practise if it does in the future because it is something that can be affected by that agent.
Of course, always when we're starting a new medication, we need to make sure that we work with the pharmacist to understand whether there might be any drug-to-drug interactions for any other medications that a patient is taking for comorbid illnesses.
Jason, I wonder, how do you think the nurse can best support the patient with side effect management as he's starting or taking PARP inhibitors?
Jason Alcorn: As you'd expect me to say, I think nurses play a key role in educating patients, as we all do, about the potential side effects and maintaining them on that treatment. But I also think nurses have a key role in that we develop close relationships with our patients, very often more so than other professionals. And I think we're very good at having open communications with patients and that facilitates any detection and hopefully we can use our communication skills in monitoring the patients and picking up those possible changes even before the patients actually communicate with us. But I also think we can best support our patients by helping them help themselves, and that is always a good way of helping them to maintain a good quality of life because ultimately that's what we want. That's what we all want. And by doing that, we can keep patients on treatment for longer and manage their disease and help them manage their disease.
And all this is based in education, and we've talked a lot about education through this podcast. It's empowerment to the patient, helping the patients take control of what's going on. But having that shared decision making with everyone, the physician, the patient and the nurse all making that decision together. And I think that is a key success in keeping the patient on treatment, giving them a good quality of life and also helping them through a time in life, which is not one that they would wish for.
Alicia Morgans: I could not agree more. I think that feeling a loss of control can be so unsettling and empowering patients to understand what's happening and to actively play a role in their disease management and in the management of their side effects and in their lives is so important. So, I really agree with you there. You know, one thing that can be challenging though, with guys in general and this would include men with prostate cancer, is that they don't always really want to share their thoughts and feelings that they don't feel as open. Do you have any ways or tricks that you use to try to help guys speak more openly so that they share their side effect concerns? And they're not just trying to, you know, carry the weight of everything on their shoulders alone?
Jason Alcorn: Yeah. I think education is key and not only education for the patient, but also family members, because very often, as you just pointed out, men will feel that they need to carry the burden and not let anybody know. It is very often the loved ones that will give us that information to give us that way into getting patients to talk about the side effects. And I think as soon as you get that way in, then the patients, you know, they feel empowered that they can talk about the side effects.
And I think if you give men ways of managing the side effects themselves, they'll be more engaging and they'll be more likely to actually open up to you and ask for ways to help, you know, because then they don't feel that as though they’re putting on you or the service as much.
So, I definitely think that education is key in all this and which we've hopefully highlighted through this.
So, before we finish Alicia, I think it's worth noting that in the near future, we're going to see data from a number of ongoing trials which have investigated PARP inhibitors in prostate cancer, also in combination with other treatments. Do you have any comments about these trials and what they may mean for our patients?
Alicia Morgans: Absolutely. And we already have seen press releases suggesting that the combination of PARP inhibitors and androgen receptor-targeted agents, so agents that really stop testosterone signalling, are going to be synergistic and really these combinations are moments away, I think, from being at least considered as options for our patients. What's also really important and again, this is only from a press release so we do need to really have the full data to understand the effects here, but it suggests that these combinations may be useful in patients even when they don’t have DNA repair defect alterations in their germline or somatic settings. So, it may expand the number of patients who may ultimately be able to benefit from PARP inhibitors.
And that's why it's so important, I think that we continue to educate ourselves and educate our patients on the side effects and understanding how we can best support our patients to receive these treatments so that they can engage in combinations or other settings where PARP inhibitors may be used in the future, over time.
And then finally, I think as we do continue to understand where we might use PARP inhibitors in the future and combinations or in earlier settings of the disease or elsewhere. We, of course, have to keep our eye on the adverse event profiles and make sure that we understand, you know, whether there are new adverse events that come with combinations or patients at higher risk so that we can protect those patients and ensure that they get the right treatment for their prostate cancer, but also ensure that they have the right treatment for their comorbid illnesses or if they are vulnerable we identify those complications early.
Jason Alcorn: Well, thank you for a very interesting discussion. I've really enjoyed it and learnt some things myself. Would you like to share some key take-home messages for our listeners?
Alicia Morgans: Sure. I would just say that the adverse event profile of PARP inhibitors, I think, is quite manageable, and the best thing we can do for our patients is educate them on what to expect in terms of fatigue, cytopenia’s, maybe some GI effects, because these are generally manageable, and if they bring their concerns to the nurse team, to the doctor team, I think we can help support them to safely receive these treatments. And I would say that the future holds promise for use of PARP inhibitors, both in patients with germline and somatic mutations, but potentially even broader populations that don't have those mutations that others may benefit as well. And so all that we can do to try to keep patients safe, help them understand the treatment decision and engage in those treatment decisions will be important as we move forward.
Jason Alcorn: Well, thanks again Alicia, and I've really enjoyed our discussion. And thanks to our listeners and we encourage you to tune in to the other two podcasts in this series on PARP inhibitors in prostate cancer. Thank you.
Dr Morgans is Genitourinary Medical Oncologist at Dana-Farber Cancer Institute, and Faculty in Medicine at Harvard Medical School in Boston, MA. She completed medical school and residency at the University of Pennsylvania School of Medicine, fellowship in Hematology/Oncology at Harvard’s Dana Farber Cancer Institute and Massachusetts General Hospital Cancer Center in Boston and earned a Master of Public Health at Vanderbilt University. Dr Morgans treats patients with prostate, bladder, and testicular cancer, and her research assesses complications of advanced prostate cancer survivorship and patient-centered treatment decision-making in advanced prostate cancer.
AAA, Astellas, AstraZeneca, Bayer, Exelixis, Janssen, Myovant, Novartis, Pfizer, Sanofi and Telix.
Jason Alcorn is the Nurse Consultant for Uro-oncology and Andrology at the Mid Yorkshire Hospitals NHS Trust. He has worked at the Trust for 20 years. The Mid Yorkshire Hospitals NHS Trust is a specialist cancer centre for urological cancers. Jason started in the nursing profession after a career in the military. After completing a Bachelor’s degree developing student nurse resources, he then studied for a Master’s degree seeking to understand registered nurse understanding of delegation to healthcare assistants. This led to him being a fellow of the higher education academy and a registered teacher. He then studied for a professional doctorate seeking to understand why patients withdraw early from Bacillus Calmette-Guerin treatment for urothelial cancer. Jason has presented at several national and international conferences, as well as running workshops locally and in the Middle East on behalf of EAUN, and he has also published several articles from his research activity. He is an active board member of the European Association of Urological Nurses (EAUN) and his responsibilities on the board include education, accreditation and endorsement. __________________________
El potencial de los inhibidores de PARP en el cáncer de próstata: Lo que las enfermeras deben saber
En el segundo episodio de esta serie de podcasts, Pablo Peinado y la Dra. Elena Castro analizan los inhibidores de PARP, cómo funcionan, revisan datos clave de ensayos, cómo seleccionar PARPi y dónde encajan en la secuencia general de tratamiento.
In the third and final episode, Dr Jason Alcorn and Dr Alicia Morgans discuss adverse events associated with PARP inhibitors and the management of them, in particular thrombocytopenia, gastrointestinal effects and fatigue. Jason provides some insight into how nurses support and communicate with patients, the importance of early reporting of side effects and how to manage these. Finally, the ongoing trials of PARP inhibitors in combination with other prostate cancer treatments are also considered and what these trials may mean for patients.
Dr Morgans is Genitourinary Medical Oncologist at Dana-Farber Cancer Institute, and Faculty in Medicine at Harvard Medical School in Boston, MA. She completed medical school and residency at the University of Pennsylvania School of Medicine, fellowship in Hematology/Oncology at Harvard’s Dana Farber Cancer Institute and Massachusetts General Hospital Cancer Center in Boston and earned a Master of Public Health at Vanderbilt University. Dr Morgans treats patients with prostate, bladder, and testicular cancer, and her research assesses complications of advanced prostate cancer survivorship and patient-centered treatment decision-making in advanced prostate cancer.
AAA, Astellas, AstraZeneca, Bayer, Exelixis, Janssen, Myovant, Novartis, Pfizer, Sanofi and Telix.
Jason Alcorn is the Nurse Consultant for Uro-oncology and Andrology at the Mid Yorkshire Hospitals NHS Trust. He has worked at the Trust for 20 years. The Mid Yorkshire Hospitals NHS Trust is a specialist cancer centre for urological cancers. Jason started in the nursing profession after a career in the military. After completing a Bachelor’s degree developing student nurse resources, he then studied for a Master’s degree seeking to understand registered nurse understanding of delegation to healthcare assistants. This led to him being a fellow of the higher education academy and a registered teacher. He then studied for a professional doctorate seeking to understand why patients withdraw early from Bacillus Calmette-Guerin treatment for urothelial cancer. Jason has presented at several national and international conferences, as well as running workshops locally and in the Middle East on behalf of EAUN, and he has also published several articles from his research activity. He is an active board member of the European Association of Urological Nurses (EAUN) and his responsibilities on the board include education, accreditation and endorsement. __________________________
El potencial de los inhibidores de PARP en el cáncer de próstata: Lo que las enfermeras deben saber
En el segundo episodio de esta serie de podcasts, Pablo Peinado y la Dra. Elena Castro analizan los inhibidores de PARP, cómo funcionan, revisan datos clave de ensayos, cómo seleccionar PARPi y dónde encajan en la secuencia general de tratamiento.
Other programmes of interest
ADCs in HER2+ metastatic breast cancer and management of adverse events
Consensus-based guidance for clinicians and patients
Understanding HER2 testing in gynecological cancers
Best practices and treatment implications
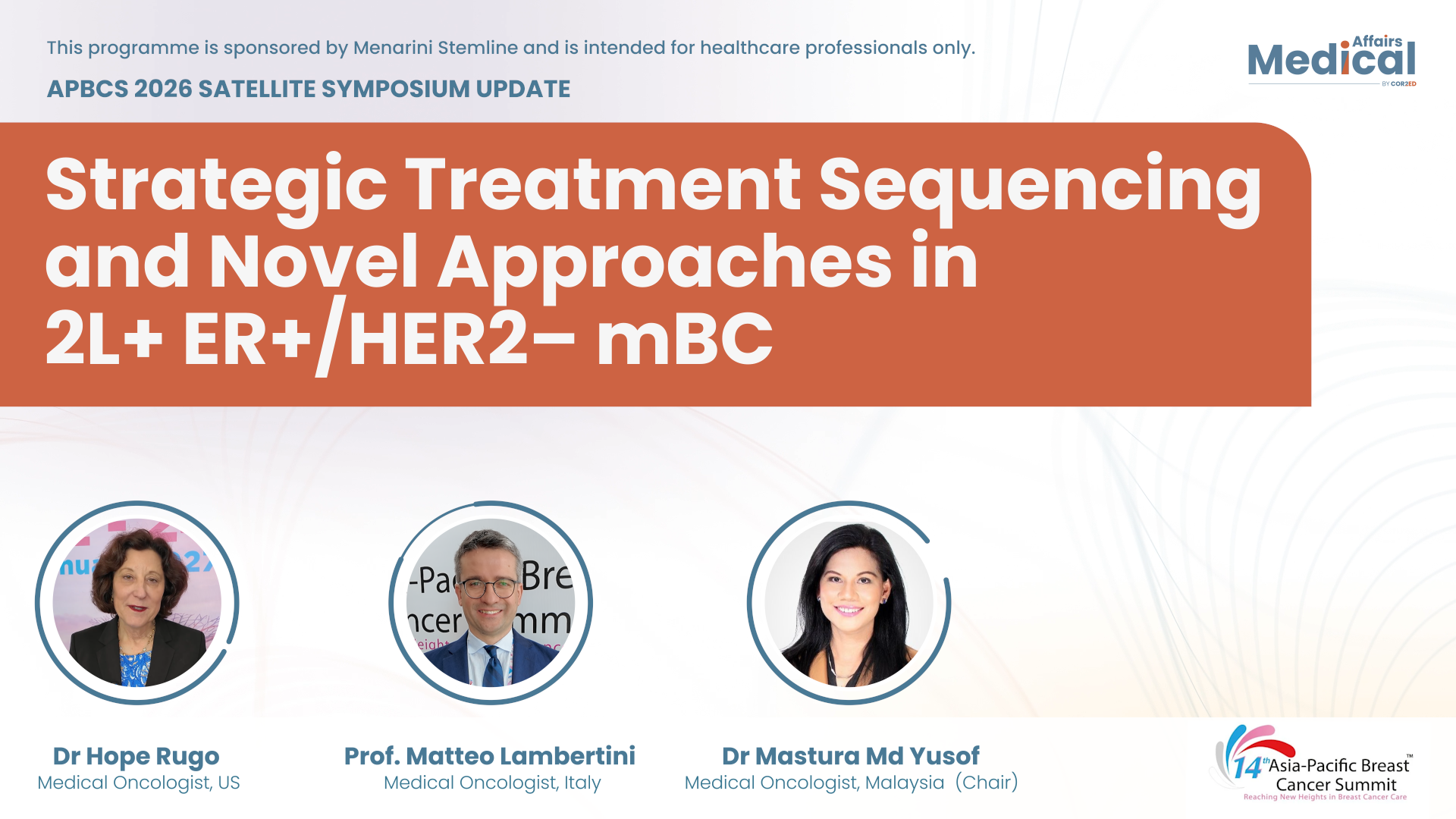
ER+/HER2- metastatic breast cancer: Highlights from the APBCS 2026 Satellite Symposium
Experts discuss 2L+ treatment strategies in endocrine therapy-eligible patients
Experts
Dr Mastura Md Yusof, Dr Hope S. Rugo, Prof. Matteo LambertiniMetastatic breast cancer: Understanding HER2-low and HER2-ultralow classification
A novel therapeutic framework
Experts
Dr Komal Jhaveri, Oncology Brothers (Moderators)Thriving beyond an EP-NEC diagnosis
Perspectives on treatment and care














 Downloadable
Downloadable  20 MIN
20 MIN
 Feb 2026
Feb 2026