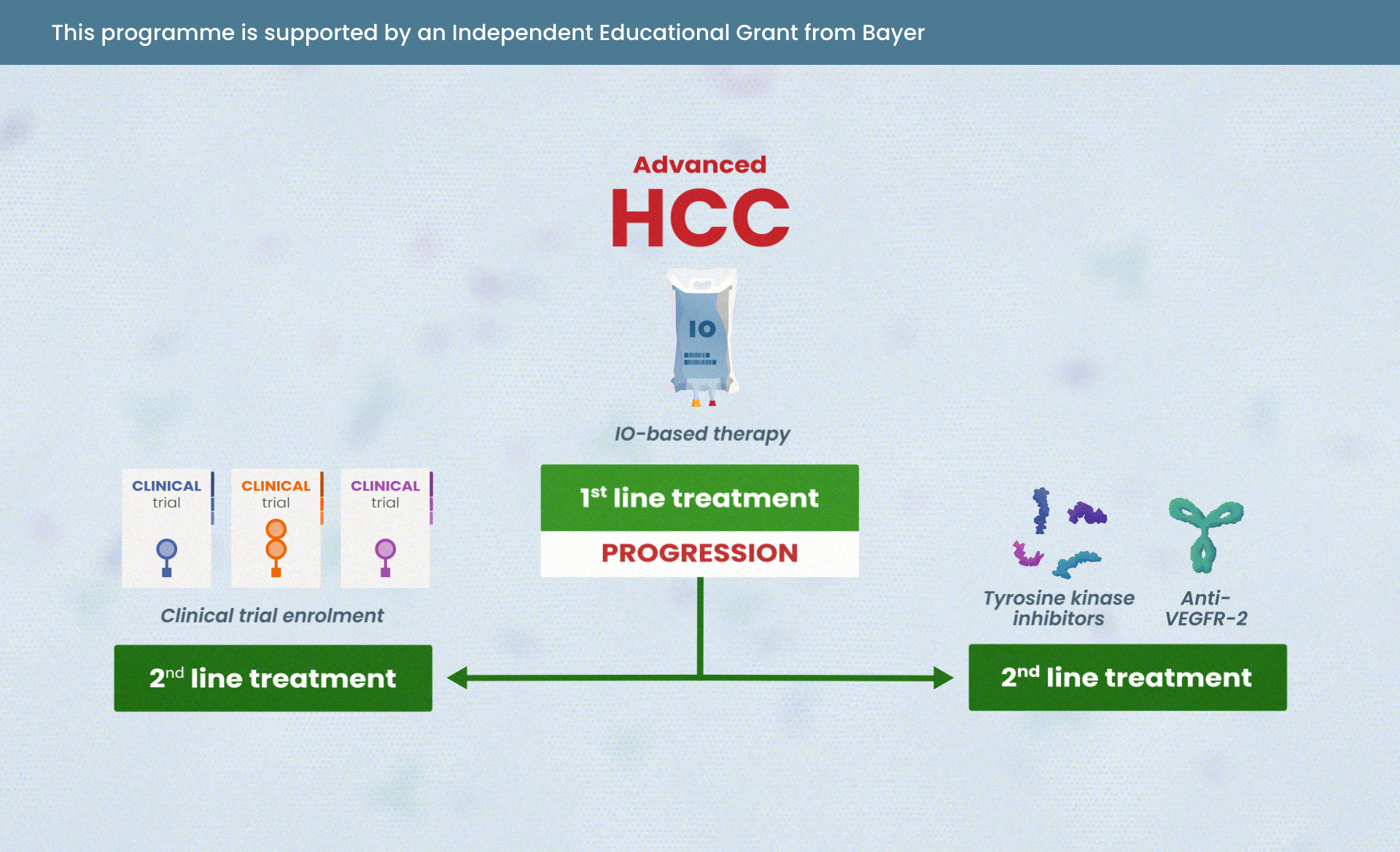
Treatment options for advanced HCC patients who are not eligible for IO first line
Dr. Tonke L. de Jong
Thank you for listening to this podcast on treatment options for patients with advanced and intermediate HCC. I am Tonke de Jong and I'll be moderating today's podcast of COR2ED independent medical education.
This podcast is an initiative of COR2ED and developed by HCC CONNECT, a group of international experts working in the field of oncology. The podcast is supported by an independent educational grant from Bayer. The views expressed are the personal opinions of the experts. They do not necessarily represent the views of the experts, organisations or the rest of the HCC CONNECT Group. For expert disclosures on any conflict of interest, please visit the COR2ED website.
I'm happy to welcome today's two experts in the field of HCC. Could you please introduce yourself, Professor Dr. Harding.
Prof Dr. James J. Harding
Thank you very much. I'm Jim Harding, a medical oncologist at Memorial Sloan Kettering Cancer Center in the United States. I focus on drug development for liver and bile duct cancers. It's currently a very exciting time for the treatment of liver cancers. Systemic therapy for liver cancer is evolving rapidly. In 2017 and before, the field only had one systemic therapy option for patients with locally advanced or metastatic disease. Now there are over ten with regulatory approvals and much of the disease is now treated with immune based therapy, and so it's an amazing time for sure.
Dr. Tonke L. de Jong
Yeah, I agree. Thank you for that clear intro. I'm delighted to also welcome Professor Dr. Saab for this podcast episode. Welcome.
Prof Dr. Sammy Saab
Well, thank you for having me. It's a great pleasure to be among you today and talking about this very important topic of liver cancer. I'm a hepatologist at UCLA. I have been in practice here for about two decades and it's been so rewarding to see this evolution of care for people with liver disease. Liver cancer is a major public health concern. The rates remain very, very high. And this is being fuelled by an epidemic of fatty liver that we've seen throughout the whole globe. Liver cancer's very special because you're not just talking about the liver cancer itself, you're talking about the soil, the setting in which it evolved. And by this definition, the treatment is really a partnership with the hepatologist and oncology colleagues.
Dr. Tonke L. de Jong
Thank you, Professor. Dr. Saab. Today's session is all about systemic treatment options for patients with advanced and intermediate HCC, with a focus on the treatment options for patients who are not eligible for immunotherapy in first line. So there's a lot going on these days in the field of HCC and I think we first need to understand the systemic treatment options for patients with advanced and intermediate HCC.
So perhaps we can start off by giving a short overview of the systemic treatment options by looking into the key clinical trials and guidelines, Dr. Harding?
Prof Dr. James J. Harding
You know, historically, the original systemic therapy that was used for patients with advanced liver cancer was sorafenib. And this is a multi-targeted tyrosine kinase inhibitor (TKI) that was assessed on two clinical trials, the SHARP Study and the Asia-Pacific study. Both of these studies confirm that sorafenib improved overall survival over a placebo or best supportive care and became the reference standard for over a decade.
In the last 5 to 6 years, we've seen a huge explosion though in potential treatment options in the first and second line. REFLECT was a clinical study that assessed sorafenib when compared to another tyrosine kinase inhibitor called lenvatinib. The end point of this study was non-inferiority and lenvatinib was non-inferior to sorafenib and became a potential option in the front line.
Much of the excitement, though, has moved towards the immune synapse and can we block immune suppressive signals in the tumour leading to an attack of the immune system leading to benefit? And the two pivotal studies on this were IMbrave150 which assessed the monoclonal antibody PD-L1 atezolizumab plus bevacizumab, an anti-VEGF antibody and compared that to sorafenib with an end point of overall survival with the intention of superiority. This study met its end point and in secondary endpoints had a higher objective response, longer PFS (Progression Free Survival) and was quite safe and tolerable. The next approach was combination immunotherapy with the anti-PD, PD-L1 therapy durvalumab plus a single priming dose of the anti-CTLA4 antibody tremelimumab comparing it to sorafenib. Within this study, there was also an arm of single agent durvalumab, but the primary endpoint was superiority for overall survival compared to sorafenib, and the combo was superior in terms of overall survival, had a higher objective response rate, similar PFS. But as we see with immunotherapy, a tail of the curve was promising. And this too now is in the armamentarium of the front line. There are several second line options that are TKI based, but you know, this is really where the work is in the frontline now. And so when we approach a patient, it really comes to a shared decision making model of cancer care where we weigh the potential risks and benefits as well as medical contraindications that might modify the therapeutic therapies.
Dr. Tonke L. de Jong
Yeah, that's a clear overview. Thank you for that. So I was wondering - now what would you do if you're going to treat a post-transplant recurrent patient with advanced HCC, Dr. Saab?
Prof Dr. Sammy Saab
That's a very good question for a variety of reasons. Number one, liver cancer is an indication for liver transplantation. And one of the challenges we have is there is a real risk of recurrent liver cancer in the new graft. So we have a number of therapies for liver cancer. The problem is that immunotherapy works by turning on the immune system. People who've had a liver transplant, and by that definition, any solid organ transplantation, are taking immunosuppressive drugs, drugs that turn down the immune system to prevent rejection. Well, if you now introduce a medication that stimulates the immune system, that could lead to rejection, graft failure and even death in the treatment of liver cancer. So as of today, 2023, immunotherapy is contraindicated in patients with liver cancer and have had a solid organ transplantation like liver transplantation.
Our first line therapy will be a tyrosine kinase inhibitor, a TKI, like Dr. Harding just discussed.
Dr. Tonke L. de Jong
Okay. And would you agree on this approach, Dr. Harding?
Prof Dr. James J. Harding
Oh, yes, absolutely. You know, there have been now some retrospective case series, one from the Mayo Clinic another from the SEER database, where some patients with solid tumour liver transplants were treated with immunotherapy and there is a high rate of graft rejection and survival seemed poor. In my practice, I absolutely agree, this is a contraindication.
Dr. Tonke L. de Jong
Yeah. And I think you touched upon this already, Dr. Saab, but why in this particular case and in other cases like this, can we not use immunotherapy?
Prof Dr. Sammy Saab
Oh, wonderful question. So in conditions and health conditions that you need to modify your immune system, suppress it like in people who've had a liver transplant, people who have autoimmune conditions, for instance, rheumatoid arthritis, lupus, people who have colitis also colitis Crohn's disease, they need a suppressed immune system for homeostasis, for lack of a better word. And now if you introduce an immune stimulator, it really wrecks things and it can cause serious underlying health problems, exacerbation of arthritis, exacerbation of autoimmune liver disease and of course, colitis.
There are other individuals also where you might not consider IO's (immunotherapy) and those who have very advanced liver disease and also those who for practical reasons, cannot be infused on a regular basis because of distance or what have you.
So there is a pretty big group of such individuals who are not eligible for IO's as first line therapy of their liver cancer.
Dr. Tonke L. de Jong
So if we would summarise those subgroups who are not eligible for IO first line, who would they be, Dr. Harding?
Prof Dr. James J. Harding
I think it would be, as we stated, the prior liver transplant, HCC recurrence, this is the primary one. I think in those patients with active or uncontrolled autoimmunity, this would be a relative contraindication. There are some data even in these subsets where you might be able to give an immunotherapy. However, you would need to do so with the aid of a rheumatologist and having their disease under control.
There are, as Dr Saab said, a subset of patients for which whomever reason may decline or be inappropriate for intravenous therapy and in those patients, a TKI would certainly be reasonable. And then in organ dysfunction, the field of IO in that space is still clarifying itself. It does appear that some subsets might be safe, but still ongoing work is required.
Date 15th May 2023: Post recording clarification from Dr Harding: note that TKIs have been studied in organ dysfunction and likewise, ongoing studies have shown preliminary safety for immune checkpoint inhibitors. More studies are needed to define the best medical approach—and these are ongoing. In some instances best supportive care may need to be considered.
Dr. Tonke L. de Jong
And for those patients, so for those patient subgroups, how do you choose the right treatment? What guidelines do you use and what do they say about these patients subgroups, Dr. Saab?
Prof Dr. Sammy Saab
We have a number of guidelines that are available in the U.S. and in Europe and in Asia. The ones that we use here are the National Comprehensive Cancer Network (NCCN)o guidelines. These are based on expert opinion. They're also based on evidence based research. And what they highlight is, as Dr Harding said, is immunotherapy, atezolizumab + bevacizumab, is a preferred regimen for most people with liver cancer, but the society also adds that it's not a one size fits all program. There are subsets like Dr. Harding and I have emphasised, that really benefit from other first line therapy. Atezolizumab + bevacizumab is not the only first line therapy and the oral TKI sorafanib and lenvatinib are also first line therapy and they play a very special role in the patient we just described. Patients who have an impaired immune system, organ transfer recipients, people with autoimmune disease and as Dr. Harding mentioned, also people who have a practical concern with IO, from distance and infusions and things are those nature.
So the National Comprehensive Cancer Network do highlight that there are a subset of individuals who benefit from atezolizumab + bevacizumab, but there are also others for which we consider oral TKIs as their first line therapy for liver cancer.
Dr. Tonke L. de Jong
That's very clear. Thank you for that. Now let's move on to the overview of the treatment options for those patients that are not eligible for IO in first line. So I'm wondering, what are the main treatment options for these patients, Dr. Harding?
Prof Dr. James J. Harding
In the subset that can't tolerate an immunotherapeutic or would not be a candidate, it's really based heavily on tyrosine kinase inhibitors. As you know, these drugs have been around for many years and have excellent preclinical data for impairing HCC and as we'll talk about, high level clinical data to improve survival and control tumours. The two that have been tested to the highest level in the first line are sorafenib and lenvatinib.
Dr. Tonke L. de Jong
And what are the main clinical trials around these TKIs? Could you tell us more about the efficacy and the safety data?
Prof Dr. James J. Harding
So Sorafenib, as stated earlier, was assessed on two trials. In the Western patient population, the SHARP study and in Eastern patient population, the Asia-Pacific study. Similar in their entry inclusion, advanced locally treatment refractory HCC, required a biopsy. Patients were randomised to receive sorafenib 400 milligrams orally BID to placebo or best supportive care. The primary endpoint was the overall survival endpoint, and in both studies, the overall survival was met. The median overall survival at that time to sorafenib was somewhere about ten months. As time has gone on and sorafenib has been a control arm on many trials, the median survival has increased over time. It's now about 14 months in contemporary studies and unclear as to why that is but nonetheless, that's what the kind of benchmark is there.
As sorafenib rarely shrinks tumours it's cytostatic, so the response rate is less than 10%. But it does delay time to progression and improves progression free survival. Its main toxicities are those seen with the TKI. Dermatologic hand foot syndrome, GI toxicity and mucositis as well as hypertension, poor wound healing. Though all manageable. That was the benchmark for many years. I do think it is being displaced now with other drugs that we'll talk about too.
Dr. Tonke L. de Jong
So what about lenvatinib Dr. Saab?
Prof Dr. Sammy Saab
I think that the data for lenvatinib is as exciting as sorafenib. The data for lenvatinib for liver cancer, unresectable liver cancer, comes from two major trials. One is called REFLECT where the authors compare the efficacy and safety of lenvatinib with sorafenib, and the other is called the LEAP-002 where the use of lenvatinib was compared to a combination of lenvatinib and pembrolizumab.
So let's look, for example, REFLECT, the study where the drug was compared directly with sorafenib. That data is compelling because what it highlighted is that lenvatinib does a very good job of slowing down disease progression. What they found was that the overall response rate was 24% and the median time to progression was 7.4 months, overall survival was 13.6 months.
Now if we now jump to LEAP-002, again when we compare lenvatinib to lenvatinib and pembrolizumab, the results were equally exciting. One of the highlights of the study was that the overall results are similar between the two groups. In other words, there was not a major incremental improvement in response when you added pembrolizumab to lenvatinib. In that study the overall survival in patients that took lenvatinib alone was 19 months. As Dr. Harding said over time these survival rates improve and when you compare the survival rate with that in the REFLECT trial a number of years ago, that was 13.6 months. Now going back to LEAP-002, again the overall survival in the lenvatinib arm was 19 months. In the combination of pembrolizumab and lenvatinib it was only a couple of months longer at 21, not significantly different. So these two trials highlight the important role we place lenvatinib in our clinical practice as a potential first time therapy.
Dr. Tonke L. de Jong
Thanks. Dr. Harding, what are the most common side effects that you see in your patients for these treatments and how do you manage toxicity?
Prof Dr. James J. Harding
The toxicity is really based on the mechanism of action of the drug. They're both multi targeted tyrosine kinase inhibitors, and they target VEGF platelet derived growth factors and others. When we look at the toxicities of sorafenib and lenvatinib actually based on the REFLECT study, the total number of adverse events or the proportion of adverse events is similar, but the types and severity of toxicity do differ and that probably has to do with how these molecules act biochemically. They are different biochemically. For example, lenvatinib’s main clinical toxicity that we see is some gastrointestinal anorexia and weight loss as well as anti-VEGF mediated toxicities such as cardiovascular, hypertension maybe quite common with the medication. Additionally, we do see some, you know, diarrhoea, stomach upset, etc. All of these have specific management guidelines.
In contrast, sorafenib tends to have similar toxicities, but has a higher rate of hand-foot syndrome where we see reddening and callousing of the hands and feet that can be quite painful and limited mobility and motion. And so really these things need to be kind of monitored and also, you know, thought about when we select patients for these treatments.
So for example, for either one of these, I do make sure we have a good assessment of the cardiovascular health of the patient. If they have hypertension, I'd like to see that controlled. We monitor that frequently throughout treatment with even home blood pressure cuff monitoring. For the dermatologic, potential toxicities I usually do a basic skin examination, prescribe emollients. There is some data for even prophylactic urea cream to prevent hand-foot syndrome, and I engage dermatology when needed. For GI toxicity there are supportive medications that might be used and I counsel patients on all of this. And of course as we monitor these patients, we do see them at a set frequency where we're checking baseline laboratories and performing physical exam to ameliorate this.
Dr. Tonke L. de Jong
I'm wondering, Dr. Saab, do you agree on that? Would you take the same approach as. Dr. Harding?
Prof Dr. Sammy Saab
Oh, undoubtedly. Dr. Harding that was a great summary of the side effects. I don't think anyone could top that. I do want to say a couple of things. You know, these drugs, they've been around for a while now and most are very comfortable with managing side effects. I like to say that the side effects are predictable. We know that sorafenib has a higher likelihood of causing hand-foot skin reaction. We know that lenvatinib has a similar but different set of side effects, mainly hypertension. So the side effects are predictable, they're manageable, and they get better with intervention. It's important that when people are on therapy, we're able to assess them or offer assistance on a regular basis. Because the sooner you intervene on a side effect, the better the outcome will be for the patient. We don't want to have a scenario where the patient has hand-foot skin reaction and doesn't want the medication ever again. And we have to make sure that we have timely intervention in our patient and see them on a regular basis. Don't wait for them to call us with a complaint, we have to be proactive. In our practice we'll see a patient 2 to 4 weeks after starting a tyrosine kinase inhibitor and then maybe monthly after that. But we play a very active role like Dr. Harding implied.
Dr. Tonke L. de Jong
Great. That's very clear. Thank you for that. So now that we come to the end of our podcast episode, what would be your main message for our listeners, Dr. Harding?
Prof Dr. James J. Harding
The main message is the field has advanced rapidly. Immunotherapy is truly a preferred regimen for many patients in the front line setting with liver cancer. The two that we've seen most data from are atezolizumab and bevacizumab, as well as the tremelimumab with durvalumab. That said, there is a cohort of patients that may not be eligible for those therapies and that could include patients who are post-liver transplant for liver cancer, those with an active or uncontrolled autoimmunity, those that just decline said therapy for various reasons and perhaps even in a poor organ status function. And so we have to keep those in mind and use all potential therapies to the benefit of patients.
Dr. Tonke L. de Jong
Thank you for this clear message. Dr. Saab would you have anything to add?
Prof Dr. Sammy Saab
Dr. Harding mentioned way at the beginning of this podcast, this is a very exciting time for us in helping people with liver cancer to hold their hand and get them through this very debilitating process. I think the overlying theme of today's podcast is it's not a one size fits all for everybody. There are subsets, cohort groups of individuals that do not benefit from immunotherapy for reasons Dr. Harding mentioned, they had a liver transplant, they have an autoimmune condition, these individuals will not benefit from immunotherapy. In contrast, we have another first line therapy. It's also effective and is also relatively safe. There are side effects, but like I mentioned the side effects are predictable and they get better with intervention. So it's a wonderful time, so we have different options for patients and to make sure we tailor management according to the patient needs as they may exist. Thank you.
Dr. Tonke L. de Jong
Thank you so much Professor Dr. Harding and Professor Dr. Saab for diving deeper into the systemic treatment options for HCC patients who are not eligible for IO in first line. I've learned a lot from your discussions, so thanks.
Prof Dr. James J. Harding
Thank you so much. This was a great podcast and I've learned so much from you, Dr. Saab, as always. Thank you.
Prof Dr. Sammy Saab
Well, thank you, Dr. Harding. This is a great podcast. I learnt a lot from this interview. I learnt a lot from you Dr. Harding, a world authority on liver cancer. And I think we all did it in advocacy of our patients with liver cancer, and we hope to continue our efforts to improve their survival and their quality of life. Again, thank you Dr. Harding, thank you everybody.
Dr. Tonke L. de Jong
Thank you. I'm really looking forward to the second episode of this series where we will discuss the right time to switch to second line therapy and enabling optimal sequencing for these patients. In the second episode, we will go through those second line treatment options such as regorafenib, cabozantinib and ramucirumab. Make sure to listen to that podcast if you want to find out more about second line treatment therapies for advanced HCC patients.
If you're interested in finding out more about HCC, then please visit cor2ed.com and select oncology. If you like this podcast, then don't forget to rate this episode or inform your colleagues about it. Thank you for listening and see you next time. This podcast was brought to you by COR2ED Independent Medical Education. Please visit cor2ed.com for more information.










 Downloadable
Downloadable  5 MIN
5 MIN
 Jun 2025
Jun 2025