Please note:
GI CONNECT podcasts are designed to be heard. If you are able, we encourage you to listen to the audio, which includes emotion and emphasis that is not so easily understood from the words on the page. Transcripts are edited for readability. Please check the corresponding audio before quoting in print.
This GI CONNECT programme is supported through an independent educational grant from Bayer and is an initiative of COR2ED.
The views expressed within this podcast are the personal opinions of the authors. They do not necessarily represent the views of the author’s academic institution, or the rest of the GI CONNECT group.
Jenny Seligmann: So hello and welcome to this podcast covering lower GI highlights from ESMO 2022. I'm Dr. Jenny Seligmann and I'm a GI medical oncologist and I'm based in the University of Leeds in the United Kingdom. Today, I'm delighted to be joined on this GI CONNECT podcast by Dominik Modest. Dominik, would you like to introduce yourself?
Dominik Modest: Hello everyone. My name Dominik Modest. I'm a medical oncologist working at the Charité in Berlin, just like Jenny, on specialised treatment of colorectal cancers. I'm happy to join.
Jenny Seligmann: Great. So today we are going to review some of the key colorectal cancer abstracts from this year's ESMO meeting. And I think, Dominik, I think it's pretty fair to say that it was a really good congress for colorectal cancers. Not all congresses are.
Dominik Modest: It was. Truly.
Jenny Seligmann: It was truly a great congress for colorectal cancer. So the main topics that we're going to cover today, so we're going to cover the NICHE-2 trial and give you some context to the new saying ‘the Chalabi plot’. We're also going to look at an interesting abstract using HIPEC in locally advanced colon cancers and also look at FRESCO-2 and the emerging story in KRASG12C mutations. Shall I start with the NICHE-2 data, Dominik?
Dominik Modest: Please go ahead.
Jenny Seligmann: So the NICHE-2 trial was run in the NKI in the Netherlands. And this was building upon the NICHE-1 trial. So the whole purpose of this route of investigation was to look at the role of neoadjuvant immunotherapy in patients with locally advanced deficient mismatch repair or MSI high colon cancer - not rectal cancer, so colon cancer. And so the NICHE-1 trial really showed some early encouraging data, not just with safety, but also efficacy. So, the NICHE-2 trial built upon that to see whether the signal that had been seen in NICHE-1, which was just in 30 dMMR patients, actually could be seen in a larger population. So the trial was now over 100 patients and the co-primary endpoints were safety and feasibility and three year disease free survival. And so what was presented in the presidential symposium was safety and feasibility and the secondary endpoint of pathological response.
So number one, in terms of safety and feasibility, I think we could all be quite convinced by that. The treatment was very well tolerated and there was less than 5% grade three events, which led to almost the vast majority of patients having surgery as planned on time within a six-week window. So that was very encouraging. I think the thing that really caught everybody's attention was the waterfall plot on response. This is something that we haven't seen in colon cancer before. So Myriam Chalabi reported a major pathological response rate of over two thirds of patients. And I'm going to use the figure here of 67% of a pCR, which is incredible. Would you not agree, Dominik? I mean, the whole place just burst into a round of applause. It was phenomenal.
Dominik Modest: Really. Yeah. Never experienced something like that. And colorectal cancer. I mean, we're used to these scenarios in melanoma or other breakthrough immunologic indications, but not in colon cancer. So it was really great to see this. And also that the patients who did not have a pCR, nearly all of them still had a major pathological response. And I think the key thing about it was only three weeks of treatment. If we just imagine the time from start of this study until timely surgery was considerably short. I think during COVID we had these time intervals, maybe in the routine care without having trial therapy, and they managed to integrate that into the short term interval. So basically, it's really, really tough to find any aspects of concern to discuss on that trial, which is a really hard job for us in this podcast! I may pull up one… Jenny, you've been heavily involved in the FOXTROT trial and I think we've been discussing the concept – or the emerging concept – of having neoadjuvant therapy in colon cancer, just like in rectal cancers over the last years. And I think one of the major issues and also aspects that were criticised heavily from surgical and also radiological societies was that pre staging is really hard in colon cancer. It's not an MRI of the pelvic region. It's hard to stage these. And I remember that the point of concern was especially MSI tumours. So having that in mind, how do you interpret the patient selection? Have they all had a tumour that was truly T4. Can we control on that? Was everybody in need of immunotherapy despite this unprecedented efficacy?
Jenny Seligmann: Yeah, I think that's some of the key questions that would come out of that. So in terms of the radiological staging, you're right, it seems to be more the nodal disease where the problem is and in MSI-high tumours. So we know that it's almost like tossing a coin in terms of calling nodes. So I'm not sure how confident you would be in their baseline radiological assessments, particularly with the N2 stage, I don't think we'll ever know the answer to that. And I think that there's a lot of work to be done in radiological staging in colon cancer. But I don’t think that that would stop delivering the whole story. I think this is going to emerge alongside the development of this whole new field, which is neoadjuvant colon cancer. And I think everyone's starting to understand that this is a field in colon cancer that we're now going to start moving to. And we need to improve the radiological staging as we're going, rather than stopping everything in its tracks because of the radiological staging. This could be done in parallel, of course Dominik, you need to then balance the risk of the treatment that you're giving versus the risk of uncertainty. And please just remember our position with adjuvant chemotherapy. We've been giving adjuvant chemotherapy - for how many years? - to a lot of patients that didn't require it. And here we've seen beautifully that this treatment is safe. So I think in turn, this is a conversation to have with the patient, but absolutely no way should that be a barrier into the progression of this extremely exciting field. So question back to you, Dominik. What would stop this being based upon the data that we have at the moment? Would you want to see disease-free survival? I mean, what do we tell our patients in clinic? Where are we going next?
Dominik Modest: Basically, I was just trying to give you a hard time in terms of finding perspectives! I think we're pretty much agreed. I think the DFS will be a challenge because as it was reported orally, there hasn't been a record of relapse yet. So I think they are on their way to have a quite convincing three year DFS rate. So basically I'm not sure whether this will change. And the median follow up, which was clearly better than the data that we had in rectal cancers at ASCO with the six months of dostarlimab, was longer than a year in contrast to 6.8 months with dostarlimab. I think the questions are quite clear. How much immunotherapy is needed for maybe those that have not reached a pCR? And the key question, of course, somehow emerging is, is that a curative therapy in itself? We cannot answer that now. I think we need the long-term follow-up data as they are now and see whether there is distant relapse. I think we are pretty much confident maybe with the rectal cancer trial to have a local control assessment and maybe extrapolate that to a certain extent to the colon where we find it increasingly difficult to monitor. So we are getting in the uncertainties here.
Jenny Seligmann: You see it as an uncertainty. I see it as opportunity. I think, number one, we can't completely extrapolate rectal to colon. I think you're right. I think we could be looking at cure in some patients, but we need to be confident that we can have a monitoring of response in the way that it's taken 20 years to get to organ preservation protocols in rectal cancer. There are none in colon cancer. Colonoscopy, of course, is going to be more difficult. Some of the flexures, you're just not going to be able to get good pictures. So yes, absolutely. But I think the next cure. Absolutely. But we need to find ways that feel safe and good ways to monitor the patients and monitor response. So I think this is, again, just opening a whole new era for personalised medicine and colon cancer, which is super exciting.
Dominik Modest: Agreeing on that, I would try to put a bit of context to emerging or maybe old stories which have a certain overlap with the NICHE trial. So I'll take a hard turn and introduce the HIPECT4 that we've also seen at ESMO. This was an oral presentation and it comes up with a quite somehow intuitive but maybe difficult question. The question of the HIPECT4 trial was in CT4 patients, so clinically T4 patients with colon carcinoma, it was randomised to do upfront surgery and adjuvant systemic therapy versus surgery plus a HIPEC with mitomycin C, 30mg per square metre over 60 minutes (to the community these details are absolutely important and this is why we mention them) followed also by adjuvant systemic chemotherapy. The primary endpoint of the trial was local relapse or local control, which was clearly demonstrated to the surprise of many colleagues. I think we can say that after many, many negative trials of HIPEC that were tested in colorectal cancer of any kind of stage and treatment situation, we also had DFS and OS, and I think it's fair to say that the initial local effect did not translate into DFS or maybe also with a small trend and absolutely not into overall survival. So basically from my point of view, we have one of the most convincing demonstrations that HIPEC does something. So there is a local effect at least on the peritoneal relapse rate. However, this is also an adjuvant therapy and I think although this is coming a bit out of the corner, I think we have to put that trial into perspective with the just discussed NICHE-2 data or what's your perspective Jenny?
Jenny Seligmann: Yeah, no, I agree. I think for these really locally advanced tumours, I mean I personally would have given them upfront systemic treatment in that situation and particularly now considering a lot of those tumours as you said were dMMR or MSI high, going straight to surgery with HIPEC is clearly not going to be the best approach. But complete kudos to the investigators. These trials are very hard to run and when the trial was set up, certainly upfront systemic treatment would not have been in their minds. But Dominik, how relevant is local control? I mean, when you think about all of the steps you need to go through to have an approved treatment in early colon cancer, should this change anyone's practice? Should we be doing this for any patients? Were there any groups that benefited more than others, do you think?
Dominik Modest: So, from today's perspective, the answer, at least my answer is clearly no. I think we miss a lot of data of that trial that we should urgently get. Most of it is dMMR or pMMR. We have not seen the data. So the key question is which proportion would have been eligible for concepts like investigated in NICHE-2. We do not have any other molecular pathology except for mucinous and signet ring cell carcinoma which I find difficult to understand why these were evaluated and MSI/MSS was not, so I think many details of that trial are still unclear and it shouldn't change our clinical practice, but it might change to some extent our perspective on HIPEC because honestly spoken when I was coming to ESMO, I did not expect this trial to show anything at all. After the experience we had with the PRODIGE trial in metastatic colorectal cancer and cytoreductive surgery, which was super negative, there was not even a small signal of anything. So basically, it does not change my clinical practice, but I think it changes my perspective on HIPEC and maybe if we are able to understand who are the like absolute 10 to 12% patients that did not relapse in the peritoneum, this may open up opportunities for the future to better select these patients. And I think we will clearly and quickly agree that this will be an MSS population or needs to be an MSS population because all the other patients also...
Jenny Seligmann: I think the other question we need to ask is can we be looking at other intraperitoneal therapies? So in ovarian cancer they do other different things. You know, there's more, rather than just one dose of HIPEC there's other methods of delivering intraperitoneal chemotherapy. Maybe if we're not seeing spectacular results with HIPEC maybe we should be continuing to think about local treatments, but maybe thinking about alternative approaches.
Dominik Modest: Okay, so we agree this does not change clinical practice. But Jenny, is there another trial that may change clinical perspective?
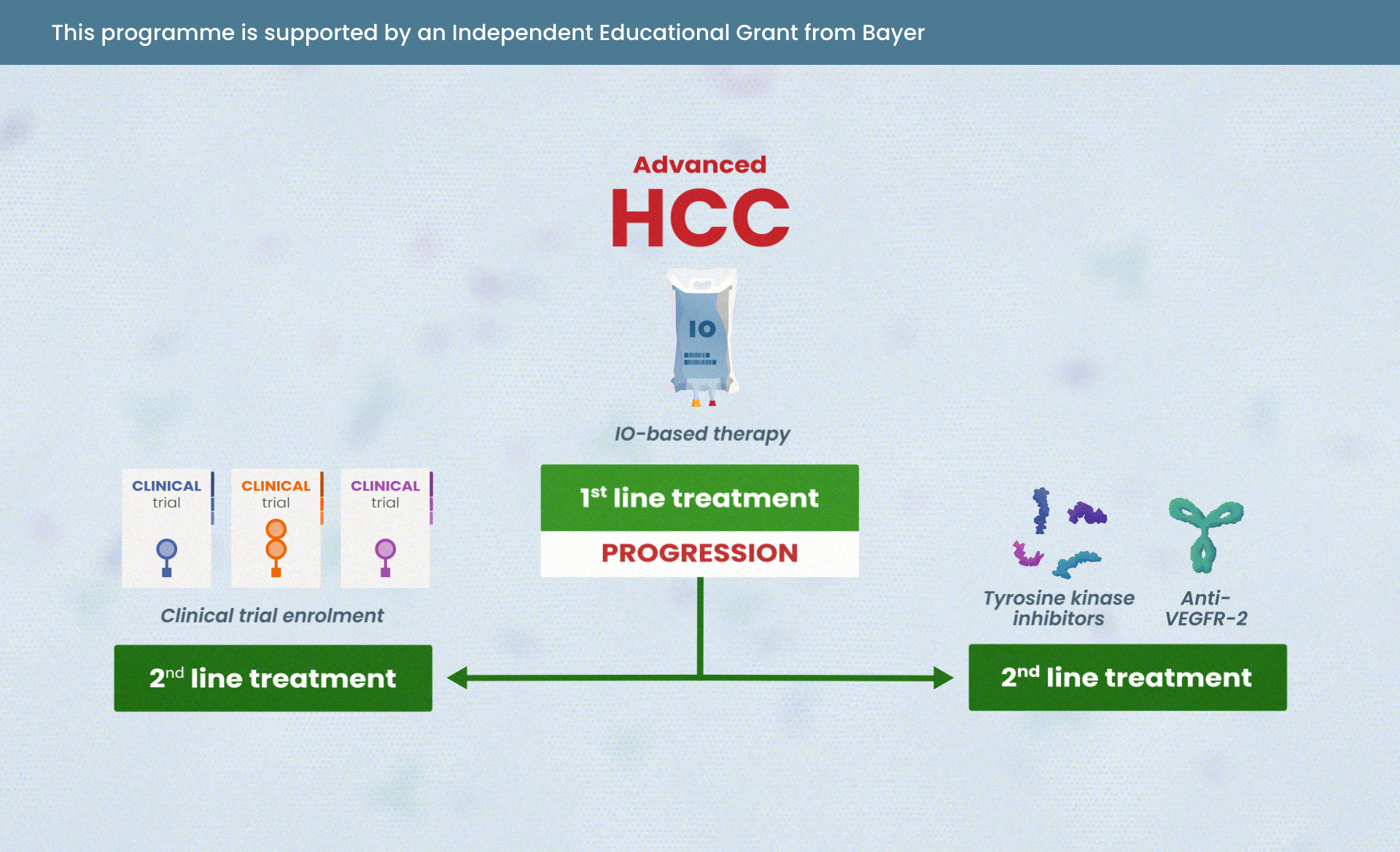
Jenny Seligmann: Well, I suppose the data that was most likely, I suppose, to routinely impact patient care would be the FRESCO-2 trial. So as you know, regorafenib is the only TKI which is approved in metastatic colorectal cancer. So the FRESCO trial was looking at fruquintinib, which is oral tyrosine kinase inhibitor of VEGF receptors 1, 2 and 3 and FRESCO-2 follows on from FRESCO-1, which had been run in China, which was testing fruquintinib in heavily pre-treated patients versus placebo but the need for another trial was felt that the standard of care in China in terms of a pre-treated patient was different from international practice. So hence the FRESCO-2 trial took place. So again, patients were heavily pre-treated and had to have had either regorafenib or TAS-102 and patients were randomised between fruquintinib plus best supportive care versus placebo plus best supportive care given the stage of the patient journey at that point. So overall survival was the primary endpoint and there was, as you can see, there was a significant improvement in overall survival, which was modest but arguably clinically significant within this population. The data are quite similar to what we had seen in other agents in this disease setting. There was a significant improvement of progression-free survival as well of around two months. The safety profile I thought looked reasonable. The main grade three toxicities were hand-foot syndrome and hypertension, less hand-foot arguably than regorafenib. So I think it was generally felt to be well-tolerated. So Dominik, what were your views? Does this now represent a new standard of care?
Dominik Modest: Yeah, I think so. At least a new potential standard of care. I think what I found a bit amazing in cross trial comparison is that the disease control rates, at least from my point of view, for the first time, was higher than 50% in that situation. We've never seen this with TAS-102 (trifluridine and tipiracil) however you call it and regorafenib, they never made it across this kind of landmark. So this was clearly better with fruquintinib. This is, I think, one aspect. The other aspect was the absolute gain in overall survival was, I think, a lucky measurement. So the hazard ratio and the gain in benefit I think is pretty much comparable to what we've seen with trifluridine and tipiracil. So that's basically, I would say, the same class of effects on the overall survival. With the toxicity I think you've summed it up nicely. However, it's a TKI, it's not so far away in terms of how the molecule is built from regorafenib, and I think we will figure out when we treat patients regularly on that drug. I expect a bit more side effects as we see with trifluridine and tipiracil and maybe a bit less as with regorafenib. And it might be somewhere in between these two drugs. And yeah, I think that's all set, it’s a new drug on the horizon. That's good news.
Jenny Seligmann: Yeah. I mean it's just one of those things, as we know, that's diminishing returns with each line of treatment. And so the number of patients that make it then to the position, if it moves forward in the patients who have had to have been treated with either TAS-102 or regorafenib if it's in that post progression population, I suppose the concern is there's fewer patients that are actually going to make it to that treatment line. So it'll be interesting to see where it is positioned eventually.
Dominik Modest: Yeah, I agree. I think if it needs now further development, I think to have trials in the third line setting are what is asked for, in the fifth line setting or sixth line setting as it was developed now because that was the patient population, I think the overall benefit for the whole population, I think we easily agree on this is considerably small. However, I think in that setting, going to third line, second line and also pre-treated patients, I think there's quite a lot of development.
Also at ESMO and I think it might get into certain clash with another kind of strategy that was emerging and I'd like to introduce at this point, which is the KRASG12C mutant metastatic colorectal cancer story. We sum up two abstracts which are basically exploring the same strategy, which is the combined inhibition of the EGFR receptor with either cetuximab or panitumumab in combination with the G12C inhibitor, which was in the one trial adagrasib and the other one sotorasib, so we have two active combinations, both were tested in pre-treated patients, heavily pre-treated patients as well, and I think the overall message was pretty simple, at least from my point of view. These combinations do work. We have a very good disease control rate, which is the vast majority of patients, above 90% in one cohort, and also objective response rates, which is beyond 30% at least, I think we can estimate from these small numbers might be even above 40% in the end. I think we have to see more patients and larger cohort to really estimate where we are. However, I think the region of objective response rate exceeds everything that we have seen as last line options, so I think there will be further development. And I think the key question, and Jenny you may comment on this, how to proceed with these combinations in the future. Where is the story leading us?
Jenny Seligmann: Sure. I mean, I think the one thing to point out is this does represent a small population of the metastatic colorectal cancer population. Excuse me if I'm wrong, off the top of my head, about 2%?
Dominik Modest: I think 3 to 4. Be a bit optimistic!
Jenny Seligmann: You're ever optimistic. Okay. So even by that, the very nature of the rare alteration does impact on the type of study design and the level of evidence that's going to be needed. I mean, it's been really nice following the story, which reminds you back to the BRAF story of the evolution of how it went. And now where we have an approved drug. Interestingly, in that setting, when we think back to the BEACON study where things have gone. So we started in the second, third line and now the interest is moving in to the first line in combination with chemotherapy. I'm very excited about seeing those patients being treated in the first line. I think you should be giving patients your most effective treatment upfront. I think we've got very good evidence that shows that depth of response to your first-line treatment has impacts all the way through. However, I suspect what we're going to end up with is a larger study again in patients who have had at least one or two lines of therapy. And it's going to really need an international effort to identify these patients and get them enrolled. And, of course, ask what the best control arm is for this group as well.
Dominik Modest: Yeah. So basically a lot of work to do. I think as you've pointed out, I think one of the major takeaways that we have is that the combined inhibition of a MAP kinase alteration together with the EGFR receptor is needed. And I would be surprised if the story would change if we get other KRAS specific inhibitors like G12D which are on the horizon. So I think for the overall strategy, how to combine drugs to find synergies, block escape mechanisms, these two abstracts were really helping us. Considering further development, I think we have to acknowledge that this is true for the BEACON as well as the now presented abstracts on G12C the efficacy of these targeted combinations is superb in terms of short term. We have super response rates and in the vast majority of patients, however, durations of response are limited. There’s evolution in the tumours ongoing and therefore I think the effort will not only be internationally in terms of how many centres that we need to recruit these patients. I also think that combinations maybe with classical chemotherapy, if you move to the first line, are needed to achieve the mentioned depth of response. Or do you have another perspective?
Jenny Seligmann: I completely agree with that. And I think unfortunately it sounds very simple, but I think even now Scott Kopetz presented more data from BEACON, again, just demonstrating the complexity with the targeted treatment. So it's not just as simple as targeting this pathway and targeting that pathway. And I think we'd be naive to go into future development thinking it's going to be quite as simple as that. So exciting times. So I think we'll sum up there. I hope you agree that this has been a really exciting time for colorectal cancer. It's been a really good conference. Thank you, Dominik, for sharing your perspectives and I hope everyone has enjoyed this GI CONNECT podcast.
Dominik Modest: Thanks a lot, Jenny. It was a pleasure.














 Downloadable
Downloadable  5 MIN
5 MIN
 Jun 2025
Jun 2025